Category Archives: How We Help
← Previous postHelpful Resources
July 22, 2014Partnerships
Caring Voice Coalition has partnered with LegalShield to offer CVC patients discounted legal plan membership. For a small, flat monthly fee, CVC patients can become LegalShield members, with access to services including unlimited legal advice on any topic, living wills, estate planning, health care proxies, insurance coverage, and identity theft protection. With LegalShield, CVC patients have access to caring, top-quality attorneys from highly-rated law firms across the country at very low cost.
NeedyMeds, founded in 1997, is a non-profit information resource devoted to helping people in need find assistance programs to help them afford their medications and costs related to health care.
Patient Associations
- Alpha-1 antitrypsin deficiency
- Ankylosing spondylitis
- Bile acid deficiency
- Chronic granulomatous disease
- Complex partial seizures
- Cutaneous lymphoma
- Factor XIII
- Gaucher’s disease
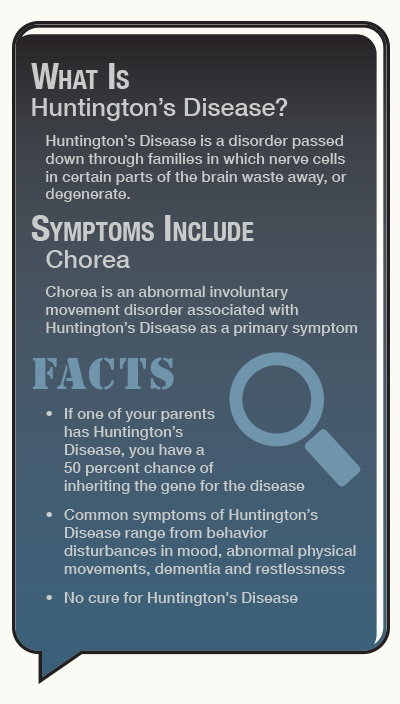
- Huntington’s disease
- Idiopathic pulmonary fibrosis
- Infantile spasms
- Lennox-Gastaut
- Lupus
- Multiple sclerosis
- Myositis
- Narcolepsy
- Nephrotic syndrome
- Orthostatic hypotension
- Psoriatic arthritis
- Pulmonary hypertension
- Rheumatoid arthritis
- Juvenile rheumatoid arthritis
- Sarcoidosis
- Stevens-Johnson syndrome
- Thalassemia syndromes
Copayment Assistance Organizations
- The Assistance Fund
- CancerCare
- HealthWell
- Leukemia and Lymphoma Society
- NORD
- Patient Access Network Foundation
- Patient Advocate Foundation
- Patient Services, Inc.
Government Agencies and Programs
- BenefitsCheckUp
- Medicaid
- Medicare
- National Institutes of Health (NIH)
- Social Security Administration
Transplant Information
Posted in How We Help | Leave a commentUnderstanding Your Disability
April 28, 2014Many persons impacted by a chronic illness reach a point where they can no longer work. To help allow for continued income and insurance, Caring Voice developed a Disability Program to help individuals understand the complicated issues involved in proving entitlement for disability benefits. By providing accurate information about Social Security programs and the benefits that you and your family may be eligible for, CVC provides guidance in determining whether applying for disability is right for you.
Posted in Featured, How We Help | Leave a commentMay Is Huntington’s Disease Awareness Month
May 9, 2013Jean Wittie shared her story with us back in November of 2012 for our special edition of Community magazine, In Their Words. Her story detailed how Huntington’s disease has affected her family. Below is her story.

Jean Wittie, directly right of the groom, with members of her family on the Oregon Coast
My husband Frank and I have been married for over 30 years. We have a blended family of seven children, six grand children and five great grandchildren. The two oldest boys are my boys from my first marriage, and they are the ones who have been diagnosed.
Todd is the younger one, he’s 43. He began having some problems – facial twitching and jerking – in 2009. He’d always had problems with his thyroid, and his doctor at the time thought all of Todd’s problems were related to that. The doctor kept raising and raising the medication, until he took Todd completely off it. Nothing worked.
I finally took him to my doctor, who thought he had MS. We went to see a neurologist who ordered an MRI and genetic tests. When the diagnosis came back, it blindsided us. We had no idea that there was anything like this anywhere.
 After Todd was diagnosed, his doctor ordered testing for Todd’s older brother, Dale. Dale had some symptoms, but they weren’t very pronounced, so he thought he was home free. But just before Christmas 2010, his diagnosis came back as positive for HD.
After Todd was diagnosed, his doctor ordered testing for Todd’s older brother, Dale. Dale had some symptoms, but they weren’t very pronounced, so he thought he was home free. But just before Christmas 2010, his diagnosis came back as positive for HD.
So I set out to learn as much as I could about Huntington’s. I found the UC San Diego Autism Center of Excellence and they were so encouraging. They invited Todd and myself to their research symposium, where we met researchers, officials with the Huntington’s Disease Society of America, and families with HD. It was all very encouraging.
As a result of that symposium, we were finally able to get both Todd and Dale on a medication that helped restore their quality of life.
Dale lives in his own home with his adult son, daughter and her family. Dale’s daughter and her family moved back to Oregon to be closer to Dale and help out.
Unfortunately, Dale’s daughter was diagnosed positive in March. Dale’s son, and Todd’s two daughters have not yet been tested. Todd’s two girls live in Alaska and want to be tested but they are working their way through the state’s medical system now. Dale’s son is practicing avoidance behavior – he’ll get to it, but for right now, he does not want to be tested.
My husband Frank has always been supportive of the boys and of me. He’s the one that keeps reminding me to be patient when I need to be.
 I still work and I go to school, so Todd is at home alone during the day. I make meals that will be easy for him to eat, he takes care of the yard, feeds the dogs… both my husband and I want Todd to have as normal a life while he still can.
I still work and I go to school, so Todd is at home alone during the day. I make meals that will be easy for him to eat, he takes care of the yard, feeds the dogs… both my husband and I want Todd to have as normal a life while he still can.
Our extended family is huge, and Todd and Dale have all of the love and support our family can offer. Various family members have attended the conferences, support groups, walks – everyone in the family is there for Todd and Dale.
I truly feel that if I stay positive and persevere, then there will be a cure. We all have to have the courage and the hope to keep going. You have to keep fighting.
So that’s my story.
This article first appeared in the winter edition of Caring Voice Community magazine.
Posted in Diseases, Featured, How We Help | 1 CommentDo I Need a Power of Attorney?
May 1, 2013 A question CVC is often asked is whether or not patients need a Power of Attorney (POA). But before I can answer that, I’d like you to understand what a POA is and whether one is appropriate for you.
A question CVC is often asked is whether or not patients need a Power of Attorney (POA). But before I can answer that, I’d like you to understand what a POA is and whether one is appropriate for you.
What is a Power of Attorney?
A Power of Attorney is an agreement between two people: a principal and an agent. The principal, or almost always the patient, grants powers to the agent, or the caregiver, to make certain decisions on the patient’s behalf. These decisions can be based upon a range of issues, but they are typically financial or medical decisions. A POA steps in when the patient is no longer able to make decisions on his or her own behalf, and it allows the caregiver to designate who will make those decisions. Without a POA, a court or state may be able to designate someone to make decisions on the patient’s behalf. The person appointed might not be the person the patient would choose to make his decisions.
As an example, married couple John and Peggy choose to draft durable Powers of Attorney granting one another the authority to make financial and health care decisions on one another’s behalf. John discovers that he is diagnosed with Huntington’s Disease and eventually loses capacity to make decisions on his own. Because of the POA, Peggy can make decisions for John. Without that POA, their home state of Idaho could determine that Peggy is not the best person to make those decisions and instead designate John’s cousin, Nell, to make those decisions.
Do I need a Power of Attorney?
Probably. Most people who own property or have any money will need to make financial decisions, or difficult health care decisions later in life. If this is the case for you, you may want to consider having a POA in place.
The Specifics
When you draft a Power of Attorney, you must have the capacity to do so. Capacity is essentially the ability to make or enter into a legal relationship the same way someone with a sound mind would. Everyone is assumed to have a sound mind and be of normal intelligence. Someone can try to prove that you no longer have capacity. However, to do that, they must have specific and realistic proof.
So, if your illness is expected to progress in a way that may cause you to lose capacity, it is better to draft a POA sooner rather than later. You can speak to an attorney about tactics like videotaping the signing, getting one or many doctors’ statements of your competence, and/or having multiple witnesses at the signing of your POA to further support your capacity.
A POA must be durable to last after a patient loses his capacity. A durable POA will remain intact after the patient is no longer able to enter into legal relationships. A POA will terminate at death, even if it is durable.
The laws that govern Powers of Attorney vary state by state. Many people will need separate POAs for health and financial issues. Consult an attorney in your state to answer any specific questions you have and to draft a POA for you. If this is not financially possible for you, many state Departments of Health have free Medical Powers of Attorney or Health Care Proxies available through their offices. Contact your local Department of Health to request a copy of their form and for any specific instructions to complete.
If your family does draft a Power of Attorney, please send a copy to CVC. We can keep it on file in case the caregiver must sign on behalf of the patient when completing a new Terms and Conditions form or the incredibly important Renewal to receive a grant in
the new year.
The information presented in our website’s “Legal Corner” section is intended to provide information of general interest to the public and should not be relied upon as legal advice or counsel. This information should not serve as the basis for any legal decision by you. The information offered is not intended to create an attorney-client relationship, and your visit to our “Legal Corner” shall not be deemed to create such a relationship. Information posted in our “Legal Corner” may not reflect recent legal developments or decisions and therefore website visitors should consult an attorney if you have legal issues requiring attention.
Posted in Caregivers, Diseases, Featured, How We Help | 2 CommentsLiving with Chronic Granulomatous Disease (CGD)
March 1, 2013Twin boys Easton and Owen Jouppi were diagnosed with CGD a week before their first birthday. Here, the boys’ parents, Nicole and Mike Jouppi, discuss what it means to care for two children living with this chronic illness.
Their story, in their own words.
We had Owen and Easton on May 21, 2010 and on April 14, 2011 just a month before their first birthday, they were both diagnosed with CGD.
They weren’t meeting milestones that typical infants should meet. They weren’t gaining weight or eating food. There was a very clear failure to thrive.
Owen developed perirectal abscesses, and that’s something that males with CGD will get. Sometimes they will have cysts on their legs and arms, or have reoccurring pneumonia. About a month later, Easton began getting the abscesses too. Owen would lose weight as quickly as he gained it. Our pediatrician referred us to a gastrointestinal doctor who monitored Owen for a couple of months and after trying a few medications, the doctor ordered the CGD test.
They ordered the test on Easton as well because the two are identical, and the thought was if one of them has it, they both might. And they both did.
A few months later, the boys had eye surgery and the gastro doctor ordered an endoscopy and a colonoscopy. After that, we found out they not only had CGD, but chronic colitis as well.
If males get chronic colitis in addition to CGD, they don’t typically get it until later in life. Owen and Easton were 13 months old.
In CGD, the white blood cells don’t work properly. A white blood cell encases an infection and breaks it down, their white blood cells encase the infection, but do nothing with it. So infections get bigger and bigger. Basically, their bodies can’t fight off bacteria or fungal infections, so they can’t be in sandy environments, dirty areas, things like that. They don’t have to live in a bubble, but they need to be very careful.
Males have an XY chromosome and females have an XX chromosome. Females don’t get CGD often because they can cancel out the bad X, but because males have the XY chromosome, they are more at risk. After the boys were diagnosed, we learned that Nicole had been the carrier of the CGD, and she had gotten it from her mother. CGD is typically inherited through the mother, so it made sense.
The way we understand it, if a female has CGD, then her mom and dad both were carriers of it, but for males, only the mother has to be a carrier.
One of the things is that if you and I get sick, we show it on the outside. But if they’re sick, they look healthy as can be. Completely normal on the outside, but very sick internally.
Because the boys aren’t old enough to fully understand the disease, they have to be monitored constantly, which can make day care and play dates difficult. If a two and a half year old sees a kid playing in the sand, then they want to go play in the sand with them. Owen and Easton can’t do that.
Nicole actually ended up quitting her job so she could stay home with the boys full time. We realized it was going to be too difficult to put them in day care. There are the many safety precautions, but also several steps for the medication as well. It’s a very strict regimen.
We still hold out hope that they will be cured, but the only cure is a bone marrow transplant or stem cell, which is not highly recommended unless you become seriously ill. But we remain hopeful for the future.
But after all of this – the medications and safety concerns and so on – Owen and Easton are just two boys. Two boys who like to chase each other around, play with toy cars. They love going to the playground, but just have to be a little more careful than some of the other kids. It’s great to finally see them healthy and just acting like little boys. For such a long time it was such an uphill battle and struggle for them. And although we’re still learning about what they can and can’t do, it’s nice to see boys being boys.
Click here to learn more about CGD.
Posted in Diseases, Featured, How We Help | 12 CommentsPatient Education
February 28, 2013A primary goal of CVC is that, simply put, we are here to help. We understand what it means to live and cope with a chronic illness. Our patients often experience fear, confusion, frustration, anger – any number of emotions that prevent them from making the best decisions for their physical well-being. Our Patient Education program identifies public and private services to benefit our patients’ physical and emotional comfort. We connect patients and their loved ones with services that make life easier.
Posted in How We Help | Leave a commentSSDI/SSI
February 28, 2013Our SSDI/SSI programs are supported by several patient advocates who assist patients with various stages of the application process. Our patient advocates request patient medical records, assess eligibility to apply for disability benefits, review and analyze complex medical documentation, draft arguments to support the disability claim – anything to further facilitate and mediate communication between our patients and various government and health care entities.
Posted in How We Help | Leave a commentTherapy Appeals
February 28, 2013Our Therapy Appeals program exists solely for CVC to act as an advocate for our patients. If an insurance company denies coverage of a medication, and a patient is unaware of their options, CVC’s Case Managers step in to assist that patient. We coordinate supporting evidence for appeals processes, draft persuasive arguments to the insurance company to appeal the denial, and follow through – essentially, whatever it takes to get the patient’s needed therapy in their hands.
Posted in How We Help | Leave a commentAlternate Coverage
February 28, 2013Patients seeking our assistance often have trouble finding affordable insurance plans, or may encounter insurance requirements they are unable to resolve. CVC’s Insurance Specialists investigate, review and explain current benefits to our patients. We work with all insurance types – including commercial, government, and exchanges – to resolve issues and assist patients in identifying and exploring sources of new or improved coverage.
Posted in How We Help | Leave a commentUniting Behind the Zebra for Early Diagnosis of PH
December 3, 2012by Mollie Katz, Vice President, Community Engagement, Pulmonary Hypertension Association.
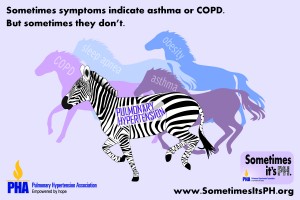
Since last June, zebras have been the hot new symbol of pulmonary hypertension (PH).
PH patients, families and caregivers around the world have rallied behind the zebra,
building its stripes into their fundraising events, posting photos of themselves in zebra
clothing and talking about the zebra in media interviews about PH. At conferences of
PH-treating professionals, zebra-striped buttons are being given away and participants
are buzzing about “the zebra campaign.”
Why?
 Among doctors, the zebra is a metaphor for an unexpected diagnosis. That’s why the Pulmonary Hypertension Association (PHA) has made it the symbol of a new 5-year initiative on the importance of considering a PH diagnosis early on. The campaign, Sometimes it’s PH, responds to a major problem — frequent misdiagnosis — by teaching health care professionals to suspect PH, screen for it and team with PH specialists to provide the best possible care.
Among doctors, the zebra is a metaphor for an unexpected diagnosis. That’s why the Pulmonary Hypertension Association (PHA) has made it the symbol of a new 5-year initiative on the importance of considering a PH diagnosis early on. The campaign, Sometimes it’s PH, responds to a major problem — frequent misdiagnosis — by teaching health care professionals to suspect PH, screen for it and team with PH specialists to provide the best possible care.
The zebra image strikes physicians immediately, because it comes straight from
their medical education. When they first learn how to reach a diagnosis, they are
taught, “When you hear hoof beats, think horses, not zebras.” In other words, doctors
learn to assume that common symptoms suggest common diseases. But with a rare
disease like PH, widespread symptoms such as shortness of breath, chest pain, fainting
and fatigue point to a “medical zebra,” similar to a horse, but very different.
Sometimes it’s PH pairs the zebra with this message to medical professionals:
Sometimes shortness of breath, chest pain and other symptoms may lead you to
conclude it’s asthma, COPD, obesity or lack of fitness. But sometimes it’s not.
Sometimes it’s PH.
The campaign aims to eliminate misdiagnosis of this illness, whose symptoms are often mistaken for other diseases. Many patients are misdiagnosed repeatedly over several years. Research shows that almost 75 percent of patients have advanced PH by the time they are diagnosed. That number has scarcely changed since the 1980s. While continuing to work toward a cure, promoting early diagnosis is PHA’s next big priority for improving patient care.
Sometimes it’s PH, led by PH-treating professionals, will educate other professionals
about PH, starting with primary care providers, the first ones patients turn to with symptoms, and later reaching specialists and likely patients. PHA will highlight its own educational programs on early diagnosis; pursue new educational programs outside PHA; communicate through medical journals, media coverage, and more; and it will connect with other groups of medical professionals to carry the early diagnosis message to their members.
Already PHA has highlighted early diagnosis in the summer issue of its medical
journal, Advances in Pulmonary Hypertension; made it the theme of its successful
PH Awareness Month in November; and has offered a webinar for professionals and
patients on the subject during PH Week at the American Thoracic Society. (The journal
and webinar will be archived at www.PHAOnlineUniv.org, PHA’s hub for medical
education, if you’d like to catch it.)
Want to unite with others behind the zebra? Show you endorse the campaign at
www.SometimesitsPH.org. Share your own misdiagnosis stories and zebra photos
there. The site also lets you view a 1-minute video spot and gives tips on sharing it
through social media. Every step strengthens our cause.
Cindy’s Story
October 19, 2012I have had a long history of coronary heart disease so it is not uncommon for me to experience angina on a regular basis. However, in November 2009 it became stronger than usual and my doctor ordered first a stress test, then a heart catheterization. The doctor preforming the cath found no real changes in the left side, so he decided to do a right sided cath and check the pulmonary artery pressure, which was elevated but not too high. He told me that I was begining to show signs of pulmonary hypertension.
I was not familiar with this and when I went to the follow up with my doctor he put me on a new medication which I assumed was for the PAH. It wasn’t, so in September 2010 I had to go to the ER due to severe angina again. Another heart cath was done including a right sided one to further assess the pulmonary pressure. It had gone from mild to severe in less than a year with a pressure of 80.
I discussed this with my doctor and asked why the new medication had not worked and I was then told that the medication he put me on was not for the pulmonary hypertension. I asked why he had not addressed the PH and he shrugged and left the room. It was at that time that I found a new cardiologist as well as a pulmonologist who put me on PH meds. I was on the lower dose for a year and a half and there were episodes of shortness of breath and I asked about possibly increasing the dosage, but the doctor did not want to do that. I had planned a trip out of the country for vacation and the doctor did a HAST test and said I was fine to fly without oxygen.
He was wrong. I thought I was going to die the enitre trip. I became very sick and really could not participate in my own vacation. By the time I got home I was even sicker. I went to the doctor to explain what had happened and he said it was not from the PH and that I should talk to my cardiologist. It was at that point that I looked for a PH specialist that my insurance accepted and found one in my general area. He is still in the process of adjusting my medications and has done two cardiac caths, one right side the other left side. I have still not been able to return to what I was able to do before the trip and the doctor isn’t sure if I will ever be able to.
When I was put on the PH meds, I had no idea how expensive the medication was and when they told me what my co-pay was I said, “Well they might as well shoot me because there is no way that I can afford that as I am on disability.” It was then that the speciality pharmacy referred me to Caring Voice. They made everything so easy and within only a couple of days had me approved for the balance of that year as well as the following year. I cannot thank them enough for making such a difficult time easier as I don’t have to fight to get my medication.
So that’s my story so far. I am still working on getting back to where I was before the trip and I am determined that I will do so. I will just have to take baby steps, but I know myself, and I will get there.
Posted in Diseases, Featured, How We Help, Media Center, Uncategorized | 1 CommentRosemary’s Story
September 21, 2012I was diagnosed with Pulmonary Hypertension November of 2011. The years before that, I was very active. I had earned a Masters Degree in Counseling in 2006, the same year I was diagnosed with asthma. I have since learned that Pulmonary Hypertension is often misdiagnosed as asthma. Despite the diagnosis, I worked full time, took care of my parents, my nephew, and I worked with horses, caring for them and cleaning up after them. I was very physically active, constantly going somewhere or doing something.
Then I started getting tired having more “asthma attacks”. I couldn’t seem to catch my breath. I started sleeping more and becoming less active. I told my doctors that I thought something was wrong with me, but they said, “There is nothing wrong with you. Exercise more, take vitamin D and lose weight”. I knew something more was wrong, but I did what they said.
I forced myself to start doing everything again, despite the exhaustion. I joined a gym and went swimming every single day and changed my diet. I could only eat a yogurt and six crackers twice a day – anything more than that and I would get sick and start coughing badly. I did lose weight but my ankles and legs were swollen from retaining water. I started going to the doctor or ED at least once a month because I couldn’t breathe. I stopped losing weight and started retaining water so badly that I could not put on my shoes.
They said, “It is nothing, just your asthma” and gave me more asthma meds. In July of 2010 the doctor diagnosed me with COPD. I asked to see a specialist, but he refused to refer me, stating the treatments for asthma and COPD were the same. I started having chest pains and my legs were so swollen they were often purple. Again, I was told to lose weight. I no longer had the energy to do anything besides go to work and come home and sleep. I was now going to the ED or my doc 2 to 3 times a month because of the chest pain and shortness of breath, swollen ankles, anxiety attacks, lack of energy and the cough.
I was given a nebulizer and a pat on the head and told to lose weight and get more active. I said “there is something very seriously wrong with me, this is not right”, but no one listened. On Nov 5th, 2011 I was taking a shower and felt a stabbing pain in my right lung – it literally knocked the wind out of me. I could not breathe and it lasted for several seconds. I finally caught my breath, did a nebulizer treatment and went to work. People kept asking if I was alright as I had lost my voice and was coughing every time I moved. I said “it’s just my asthma acting up”. The next day, I went to work and it was a blur – I was in pain, having a hard time catching my breath and then having to stop every few steps to catch my breath. That night I could not sleep because every time I laid back I couldn’t breathe and was coughing constantly.
I went to work the next morning and was only there for three hours before I saw that my fingers had turned purple and again I couldn’t catch my breath. My chest felt like it was on fire and I felt like I was going to die. I told my boss, who told me to go to the hospital or call an ambulance. As soon as I walked in the door of the hospital, the nurse at the check in took one look at me and called out “We need a wheelchair. Shortness of breath”! They took me right back to a room and were undressing me and hooking me up to machines. I was told that I had a blood clot in my right lung and I was being admitted to the hospital.
They sent me to a regular floor, however the nurses there refused me, saying I was to unstable I needed to be an a more acute unit. So, I was sent to the PCU. I told the doctor, Dr. Dexter what had been happening and he said “I don’t think this is just a blood clot, something else is going on”. I asked “Does that mean you are going to discharge me?”, to which he replied, “No, you are not leaving until I know what is wrong with you”. I was on oxygen and hooked up to IV’s, but for the first time in months I was not scared – - someone was finally listening to me. Later, I learned the doctors and nurses were wondering how I was even alive my oxygen was so low. If I had not been talking they would have put a tube down my throat to breathe for me. They said I should have been dead.
Dr. Dexter consulted with Dr. Filner, a pulmonologist before both of them said they felt I had something called Pulmonary Hypertension. Over the course of the next three weeks I was given every test imaginable. Dr. Filner requested a right heart cath, but since it was the day before Thanksgiving the cardiac team did not want to do it. They said it could be done as an outpatient, but thankfully Dr. Filner was insistent. As I was on blood thinners for the blood clot, I had to have a plasma transfusion to slow down my clotting time.
At this time a nurse said I should be discharged since my oxygen level was now at a 100 percent. “I am going to go talk to Dr. Filner about discharging you. We need this bed for really sick people and you can take off that oxygen – you don’t need it”. So I took off the oxygen and watched my numbers drop from 100 percent to 90 percent to 85 percent. The nurse almost immediately returned, very red faced, and put the oxygen back on me saying, “I guess you are staying”. He left and I did not see him again.
Soon thereafter, I had the right heart cath procedure done. At first all the doctors and techs in the room were joking around, talking about what their plans for the holidays were. But then when the surgeon performing the test said “Ok we are in, oh look at this” all of the sudden people got serious and stopped talking. They were asking if I was ok, adjusted my oxygen mask, hooked me up to more wires. The surgeon came around to see my face, laid his hand on my arm and said, “The pressure in your lungs is 80. It is supposed to be four.”
It wasn’t until Dr. Filner came and saw me and told me it was confirmed that I had Pulmonary Hypertension and I would have to quit my job and take meds for the rest of my life. I stopped listening at “quit my job”. I was at the top of my career, I was opening my own office… quit? Never I had worked so hard and long to get were I was. I didn’t hear a word he said as he was explaining things. My boss sent over paperwork for FAMLA which she said would protect my job until I came back. My co-workers took up donations for PTO and money to help my family, as I was out of my own PTO. I was discharged without oxygen and a with a whole lot of new meds.
Three weeks later I went to see Dr. Dexter’s wife, who was considered to be the best when it came to Pulmonary Hypertension. In her office they tested my oxygen levels and she immediately put me back on oxygen. She then told me I would have to be on oxygen 24/7 from now on. I tried going back to work, even though Dr. Dexter said it was not possible, which unfortunately proved to be true. Every time I tried, I was back in the hospital for at least a week. The longest I made it was when my schedule was dropped to 5 hours. I made it for three days but on the fourth, I slept through the day and couldn’t be woken up. I ended up back in the hospital for a month.
That is when I threw in the towel. I told my supervisor who advised me to talk to HR and apply for the life insurance policy. The HR Department took up another collection for me and set up a day for me to quit three days before my FAMLA was up. They did this so that if I ever wanted to work again, it would not reflect poorly on me. The HR Director also helped me with COBRA.
The company raised enough to hold me over until the insurance started, which would match 60 percent of my salary. I was going to receive $1761. It may sound like a lot, but my mortgage and car payment alone took $1000 and COBRA took $531. The oxygen I needed was $50 and the co-pay for doctor’s appointments and meds took up the rest. I had no money for food or gas but thanks to friends and my family, we struggled through.
In August of 2012 I had to choose between making my COBRA payment or getting food for the family. I had already stopped a couple of meds because I could no longer afford them. I was turned down for state assistance because I “made too much money”. I was referred to a helpline and ended up on the phone with Caring Voice. The person who assisted me said that they could help with the COBRA payment, which meant I could now spend that money on food and gas and my other meds that I needed. It was the help I needed at a time when I had lost all hope. I was about to return all the oxygen equipment go off all my meds and drop COBRA. CVC stopped me from having to do that and basically saved my life. ‘Thank you’ just doesn’t seem enough, but it is all I have right now. My gratitude and thanks is all I can give.
Posted in Diseases, Featured, How We Help, Media Center | 10 CommentsLee Ann’s Story
September 17, 2012It was the third week that my ankles had been swollen consistently. That Wednesday, May 16, 2012 my mother and husband convinced me that an ER trip was necessary. The swelling had come and gone over the past 3 months. As a 41 year old mother of two teenagers, an asthmatic and someone who was overweight, I chalked the swelling up to being heavy. The shortness of breath had been there for years and again, I chalked that up to being heavy. Then I started to notice chest pain with the swelling and shortness of breath. That was when I realized that this might be a little more serious than I thought.
At the ER, the initial thought was that I had had a heart attack. Then blood clots then eventually, the final diagnosis… Pulmonary Hypertension. The language was not new to me or my family as my niece was born two short years ago with PH.
After a whirl of tests and a week-long hospital stay, I was discharged with little knowledge other than what I had learned from my niece. A Cardiac Cath was done and with this I was introduced to my now Pulmonary Doctor whom I love. Now the diagnosis was worse. Pulmonary Hypertension and Pulmonary Veno-Occlusive Disease.
I was told that after 5 years I would have a 50% chance of living without a double lung transplant. My world just stopped. Here we were a family of four making good money and living a great life. I had to quit my job and file for Social Security Disability. I had to deliver the news to my husband and boys that I was going to die.
Here it is four months later; I have had an open lung biopsy and have been taking medications that make my symptoms worse. The money situation is so bad, we’re making enough barely struggle by, but not enough to live. I was approved for disability but have a $5000 out of pocket deductible with my husband’s insurance. Not to mention copays and script costs. Disability wont start until December 26, 2012 and Medicare wont start until May 2014.
Stress is bad, I find myself crying all the time. I try to put on a happy face but it is so hard to ask for help, watch my husband come home tired from work and do housework and cook because I cannot.
Everyone keeps saying it will be ok, my question is ok for who? I have not yet learned to deal with my illness and pray that soon I will see that I can survive.
Thank you Caring Voice Coalition for all you do everyday.
Posted in About Us, Diseases, Events, Featured, How We Help, Media Center | 8 CommentsAlex’s Story
September 7, 2012I was diagnosed with pulmonary hypertension in 1998, but my story begins two years earlier. I gave birth to my youngest of three daughters in February of 1996. Immediately, I started feeling exhausted all the time. I would wake up in the morning, feed my children breakfast, sit them down in front of the television, and fall asleep on the couch. I’d wake up in time for lunch, fix them something quick, send them out to play, and fall asleep. At 5 p.m., I’d wake up, make dinner and wait for their father to come home, where I would hand him the children and say, I’m exhausted from my day, and fall asleep. This went on for nearly a year, until we moved to Texas.
I thought the sleeping was more depression, which I had been suffering with since age five. When we moved to Texas, my two older girls were of kindergarten age and I sent them off to school. My youngest daughter and I would spend the day watching television and playing on the floor. During the summer after their kindergarten year, I began passing out. I didn’t tell anyone that I passed out, because, honestly, I thought I had fallen asleep. I thought I had woken up. But I would wake up on the floor, usually with my head throbbing, from hitting it some place.
The first time I passed out in front of someone, I was chasing my daughter around and I passed out in front of my sister and ex-mother in law. I woke up to paramedics around me taking my blood pressure, and who knows what else. I refused to go with them, because I didn’t have insurance, but promised to go to my doctor the next day.
I had been seeing a doctor, and for many months, I kept telling him how tired I was, how I could feel and even see my heart beat, not to mention having to hear it at night, when all was quiet. I told him how I was fainting. He gave me an antidepressant, and each time I would go in to see him, he’d up the dose. Until one day, a year later, I fainted in front of my younger sister. She ran and got my ex-husband, who took me in to see my primary doctor.
Luckily, he wasn’t there, so we saw his on-call doctor. He listened to my heart and actually listened to me and said, “This is not in your head. This is in your heart.” I remember that day so clearly. He sent me for an echo-cardiogram and the next day, I saw a cardiologist who gave me the news. It was a month later that I saw a specialist in Houston, Texas, Dr. Adaani Frost, who, on September 6, 1998, after I had a right heart catheterization and woke up on meds, diagnosed me correctly with primary pulmonary hypertension,
I will be celebrating my 14th year since diagnosis with a bang! I found PHCentral.org first and then PHAssociation.org, and right before my divorce was final, in 2008, I found Caring Voice Coalition, without whom, I probably wouldn’t be here, or else, I’d be in a horrible financial situation!
Thank you so much Caring Voice!!! You have been such fantastic help, not just monetarily, but emotionally as well. I don’t know what I would have done without you guys!!
Posted in Diseases, Featured, How We Help, Media Center, Uncategorized | Leave a commentNew Hours at CVC
September 4, 2012 In order to provide better service to our friends across the country, we have changed our hours.
In order to provide better service to our friends across the country, we have changed our hours.
Posted in About Us, Featured, How We Help, Media Center | Leave a comment ← Previous postNew Hours:
Monday – Thursday: 9:00am to 8:00pm
Friday: 9:00am to 6:00pm