Tag Archives: CVC
← Previous postClose Up: Nicole Paulsen, CVC Events Coordinator
August 18, 2014
I always wanted to work for a nonprofit doing event planning. My mom ran a daycare when my three older brothers and I were younger. We had the best childhood growing up. In the summers, my mom planned these elaborate, fun, themed events for all of the kids in our neighborhood. We would have “Backyard Circus Day,” “Summer Olympic Challenges,” and massive scavenger hunts on a weekly basis.
My mom now works for our county parks and recreation department, where she plans community and youth programs. Throughout high school and college, I found myself working with my mom on various youth events and summer camps and truly loved it.
I love working at CVC because I get to do fun things, not only for the patients, but also for the employees. I love to plan activities that get people excited and give them something to look forward to, like monthly events for CVC staff. I also make travel arrangements for our staff to attend many of the annual patient conferences and education days.
Speaking to patients at the conferences, I’ve learned that travel with chronic conditions can be stressful. For them, making travel arrangements is a bit more involved than for most people. They have to let the airline know in advance if they’re traveling with a POC or a CPAP machine and make sure it’s FAA-approved. Each airline has a different procedure.
Some of our patients need wheelchair assistance in the airports, accessible hotel rooms, and hotel rooms with refrigerators for their medication. Narcolepsy patients with cataplexy need to have tubs so they don’t fall in the shower and hit their heads. Many of our patients have to take their medication, eat, and sleep at certain times when they’re traveling. Some have to have infusions on a weekly basis and plan their travel around that. Patients have to have prescriptions for their machines and medications on them at all times when they travel.
The relationships they form at patient education days and annual conferences can be even more beneficial than a typical vacation. They meet people with rare and chronic diseases who are exactly like them. It can be very comforting. When they’re first diagnosed, it can be very scary. They often tell me that their doctors don’t know anything about the disease. Going to education days and conferences can be quite meaningful to them.
What I think is most important for the newly diagnosed to know, is that, when they call here, they’re not going to be sent to a typical call center. Everyone here at CVC genuinely cares about what our patients are going through and will do their absolute best to help them.
CVC receives so many thank-you notes on a daily basis. Our patients take the time to pick the cards and write heartfelt thank-you notes. Reading them, you truly understand how much of a difference we have made with their quality of life, and that is very powerful.
Posted in Diseases, Featured, Media Center | Tagged Caring Voice, Caring Voice Coalition, CVC, cvc closeup, events, events coordinator, nicole paulsen, non-profit, nonprofit | Leave a commentSubscribe to CVC-e!
July 9, 2014Subscribe to the CVC-e newsletter, your free monthly email roundup of news, tips, and more, for CVC patients and caregivers. Don’t miss a single issue of CVC-e. Sign up now!
Enter your information below.
Help Others by Sharing Your Story with CVC
June 15, 2014
You can inspire others and let them know that they’re not alone when you share your story with the Caring Voice Coalition community. You can share what’s important for new patients, caregivers, and medical professionals to know about living with rare and chronic illness. And you can tell other patients how you came to CVC and what your experience has been. No story is too big or too small.
Understanding Your Disability
April 28, 2014Many persons impacted by a chronic illness reach a point where they can no longer work. To help allow for continued income and insurance, Caring Voice developed a Disability Program to help individuals understand the complicated issues involved in proving entitlement for disability benefits. By providing accurate information about Social Security programs and the benefits that you and your family may be eligible for, CVC provides guidance in determining whether applying for disability is right for you.
Posted in Featured, How We Help | Tagged Caring Voice, Caring Voice Coalition, caring voices, caring voices coalition, chronic, CVC, Disability, disability application, disability benefits, eligibility, eligible, illness, social security | Leave a commentShop at AmazonSmile & Amazon Donates to CVC
January 28, 2014Now, when you shop on AmazonSmile, you can donate 0.5% of the price of your eligible purchases to benefit the programs of Caring Voice Coalition. Caring Voice Coalition is dedicated to improving the lives of patients with chronic and rare diseases by offering services that provide financial, emotional and educational support.
AmazonSmile is a website operated by Amazon that lets customers enjoy the same selection of products, prices and shopping features as on Amazon.com. But when customers shop on AmazonSmile (smile.amazon.com), the AmazonSmile Foundation will donate 0.5% of the price of eligible purchases to the charitable organizations selected by customers.
To select Caring Voice Coalition as your AmazonSmile charitable organization, go to http://smile.amazon.com/ch/26-0058446
Shop on AmazonSmile and the AmazonSmile Foundation will donate 0.5% of the price of eligible purchases to CVC.
Caring Voice Community Magazine Subscriptions
September 23, 2013 Community magazine would not be possible without your contributions. For $10 a year, you will receive four issues of Caring Voice Community, thereby directly benefiting Caring Voice Coalition’s patient population.
Community magazine would not be possible without your contributions. For $10 a year, you will receive four issues of Caring Voice Community, thereby directly benefiting Caring Voice Coalition’s patient population.
Please fill out this form and click submit to be taken to our secure payment feature where you can pay with a debit or credit card.
Donate Now
August 20, 2013Give Financially
Caring Voice Coalition has established a safe, secure way for you to make an on-line donation. By donating to Caring Voice Coalition, you are making a difference in the life of a patient. Caring Voice Coalition and our donors have a common goal – to help as many patients as possible. The Caring Voice Coalition is a qualified 501(c)(3) tax-exempt organization and donations are tax-deductible to the full extent of the law. Our Federal EIN is 26-0058446.
Please fill out this form and click submit to be taken to our secure payment feature where you’ll be able to make a donation with a debit or credit card.
If you prefer to send your donation by mail, please send your check made payable to Caring Voice Coalition to:
Caring Voice Coalition
8249 Meadowbridge Road
Mechanicsville, VA 23116
Thank you for your generous commitment of funds. Every dollar makes a difference!
Examining the Patient/Doctor Relationship
January 25, 2013In the winter edition of Community magazine, we conducted two separate interviews with pulmonary hypertension patient Amanda Harvey-McKee and her doctor, Murali Chakinala. We asked them to individually discuss Amanda’s diagnosis, and how they’ve spent years increasing awareness on PH.
Interview with Amanda Harvey-McKee, patient of Dr. Murali Chakinala
 We did not have the easiest relationship starting out. Now, we work really well together, but it’s been eight years in the making.
We did not have the easiest relationship starting out. Now, we work really well together, but it’s been eight years in the making.
I was a biomedical research lab manager at the time of my diagnosis. At that time, not a lot of people knew what pulmonary hypertension was. We didn’t know what the treatment was (for a person who had PH secondary to a blood clot), what the diagnostics were, it was all very new. Things have changed in the past eight years, but back then, not a lot of information readily available.
At that moment of diagnosis, you’re trying to figure out what it all means, trying to define the big words – it’s a lot. And I even felt like I had an edge of other patients because I did come from a medical background, but in that field at that time, there just was not a lot of information about PH. So I started at zero like everyone else.
My primary care physical said that Dr. Chakinala was the person I needed to see. He was the expert in his field, the up-and-comer, and he was who I needed to talk to.
When I first saw Dr. Chakinala, he had a resident with him, and I fully appreciated that. But when you’re in the patient chair and not the teaching chair, it puts things into a very different perspective. It was very frustrating to me to sit and listen to them argue over pressures and counts and scores and tests and numerical values when ultimately I just wanted to know what I was supposed to do with this disease.
I left Dr. Chakinala’s office with him telling me I didn’t need to be considered for a very complicated surgery (PTE-pulmonary thromboendarterectomy) at that time. So just as I was wrapping my mind around the possibilities of a new game plan, a few days later, he called me at my home and said I needed the surgery. That completely irked me, to be honest. So after our first meeting, and that phone call, I felt really disheartened by the whole healthcare system. It added further confusion and frustration and meant that I needed to start preparing for what would inevitably be a life-altering procedure. It was too much and I went into a bit of denial. This turned out to be a mistake on my part, because Dr. Chakinala did the right thing: he went back to review everything again, seeing that my situation wasn’t straightforward. And ultimately, he was correct in the decision that I needed the surgery sooner rather than later.
I told Dr. Chakinala, “Thanks but no thanks, I’ll call you if I need you.” And after a while, I did.
I went into heart failure and knew that I needed the surgery, so I called Dr. Chakinala, told him I needed a referral and he said no problem. I’m grateful that he was still willing to take me on as a patient.
After my surgery, I started at ground zero with him. I told him I wanted to get involved with PH, and he introduced me to a few people, and we started a PH journey together, so to speak.
I became a support group leader, and he became my go-to person for any medical question or patient question. He was, and continues to be, very accessible to me. I’m very respectful of his time and status, but if I email him, he’ll get back to me right away.
I’m very fortunate to feel this level of security, just because my doctor is available when I need him. So from a patient perspective, and a support group leader perspective, Dr. Chakinala has really been invaluable to what I’m trying to do as an advocate for this disease. It’s a good relationship in that way. I had to let go of my controlling nature and have faith he was putting me first as a patient. Since then, we have open communication, where I can ask questions and voice concerns without judgment and know I’ll receive honest answers. This leads to me being more involved with my care and allowing him to help me do so. Trust, it comes down to trust.
Interview with Dr. Murali Chakinala, doctor of Amanda Harvey-McKee
 Our history as a patient and doctor has evolved quite a bit over time. When Amanda and I first met, she was already in my opinion quite sick and I thought she needed to go down a certain path in terms of treatment, which I’m sure was daunting and scary for her. But I did feel that a proven, surgical intervention was the only treatment for her.
Our history as a patient and doctor has evolved quite a bit over time. When Amanda and I first met, she was already in my opinion quite sick and I thought she needed to go down a certain path in terms of treatment, which I’m sure was daunting and scary for her. But I did feel that a proven, surgical intervention was the only treatment for her.
I met her when she was young, working, recently married – she was trying to lead a busy life and telling her she needed evasive surgery wasn’t what she wanted to hear.
So no, we didn’t really have a solid relationship to build off of. Our immediate reaction to each other wasn’t the best. And at the time, she said she didn’t want the surgery, and we ended up not communicating for about a year. When I did see her next, her health was much worse and I reiterated my recommendation and she went and had the surgery.
Her recovery was long and rocky. She nearly didn’t survive. But she kept fighting and managed to pull through rather well. Now she’s doing great, a new person in terms of how she feels and what she’s able to do. She’s extremely committed to the Pulmonary Hypertension Association cause. She’s also fully aware about how lucky she is and how unlucky other patients are, so she’s doing what she can to give back and act as a resource for patients in need.
Her and I have acted as partners in a lot of ways, in terms of her leading grass roots efforts to help other patients. She leads the support group meetings, and I try to be a medical resource for those groups. I send patients to her support groups, and she recommends patients to me from the support groups, so we really try to help each other out.
When I reflect back on all of this, I think Amanda and I would’ve done things differently, but I learned a valuable lesson. I was a young physician and I knew what she needed but I think I was a little too blinded and focused on the treatment and not thinking about what it meant to the patient and how much her life would be affected. And clearly I didn’t sense that she wasn’t prepared for that kind of news. Instead of coming on a little softer and introducing the idea while building a relationship of trust, I was more unilateral with my opinion.
The lesson I learned is that there are treatments that we know a patient needs, but as a physician, we have to respect a patient’s decisions and ways of thinking.
That’s the difference between being a doctor who has got the initials in front of their name and a healer, someone who is really trying to help the patient. We can’t distance our patients, we have to cultivate the relationship and bring them along.
Posted in Caregivers, Featured | Tagged Caring Voice Coalition, CVC | 2 CommentsStar’s Story – Pulmonary Hypertension
January 15, 2013We have a 9-year-old daughter, Zoe, who up until September of 2012 had always been healthy, active and full of energy. At last year’s first soccer practice, Zoe was having trouble keeping up. Her face was red, her eyes and mouth were a pasty white; you could see her struggling to take a full breath.
Because, I am a home health nurse, I took her vitals and recognized right away that her blood pressure was elevated, oxygen levels were low 90’s and high 80’s, pulse was rapid, etc. During this whole episode, she was talking and wanting to eat. Her vitals soon resumed to normal.
We took her to our local doctor who told us her heart sounds were not normal and that an appointment need to be made with a pediatric cardiologist as soon as possible. Zoe continued to have mild episodes as described above, so we decided to take her to a pediatrician who was unable to find anything wrong. The next week, Zoe’s oxygen level dropped to the 80’s at school, so we took her to the pediatric group again.
There we saw a nurse who was immediately alarmed and called in the doctor that was working late sick call. They listened. When we left that night, the doctor told us what she believed the Zoe’s diagnosis would be: Idiopathic Pulmonary Hypertension.
Two days later, we were at Arkansas Children’s Hospital, where Zoe was prescribed medication to help combat her illness. Day’s later, it was suggested to us that we contact Caring Voice Coalition to see if they would help alleviate some of the financial burden of the medication.
My husband and I have talked about miracles and just truly believe CVC’s assistance was our Christmas miracle. We know in some ways that we have been fortunate – years were not wasted getting a diagnosis for this horrible disease, as it is for so many. We were put in the right place at the right time to see doctors and nurses who truly listened to what we were saying happened to Zoe at times, even though they could not see it happen in the office setting. They, like CVC took the time to care enough to listen and find a way to help.
“Thank you” is not enough to describe what we feel and think, but please know we will never forget or fail to see the significance of CVC’s gift.
Posted in Caregivers, Diseases, Featured | Tagged Caring Voice Coalition, CVC | Leave a commentAvoid Three Common Caregiver Medication Mistakes
January 10, 2013Managing the wide array of medications an older loved one takes is one of many family caregivers’ primary responsibilities. But this can be a complicated task – and mistakes can happen when you least expect them.
Have you made one of the three most common medication mistakes?
Medication Mistake #1: Making Pills Easier to Swallow
Check with the pharmacist before you change a pill in any way. Certain medications given once a day, for example, are designed to have a timed release that occurs gradually throughout the day. Crushing them or cutting them in half could alter the way the drug is released, resulting in the person getting too much at once or none at all. If swallowing pills is a problem, ask the pharmacist if the medication can be provided in a smaller tablet or in a liquid form.
Medication Mistake #2: Filling a Pill Organizer Incorrectly
A 2011 study by Northwestern University’s Feinberg School of Medicine found that 60 percent of caregivers made errors when sorting medications into pillboxes, which speaks to just how complicated sorting multiple drugs with various timings for delivery can be.
Consider asking the pharmacist if he or she will sort the pills for you when prescriptions are filled. Some will do this routinely, while others will demonstrate it a few times to show you the best way to get started.
Medication Mistake #3: Storing Medications in “Typical” Places
Many people routinely store their medications in the bathroom medicine cabinet, but temperature changes and moisture levels can alter the medication once it is opened. Be sure to read the packaging on prescription medications for storage instructions.
For more information on managing your loved one’s medications, visit www.liftcaregiving.com.
Katie Gilstrap is cofounder of Lift Caregiving.
Posted in Caregivers, Featured, Media Center | Tagged Caring Voice Coalition, CVC | Leave a commentFollow us on Social Media
January 3, 2013Often accompanied with a rare disease is an overbearing sense of isolation. Our patients are often left thinking that they are alone in their fight. But as many of our active patients will attest, social networking can help curb your solitude. By logging onto our Facebook and Twitter sites, you can interact with others who have your disease. On our Vimeo site, you may find solace in one of our patient’s stories. There are others out there like you, and we’re here to bring you together.
Posted in Featured, Media Center, Uncategorized | Tagged Caring Voice Coalition, CVC, Facebook, Social Media, Twitter, vimeo | Leave a comment
Uniting Behind the Zebra for Early Diagnosis of PH
December 3, 2012by Mollie Katz, Vice President, Community Engagement, Pulmonary Hypertension Association.
Since last June, zebras have been the hot new symbol of pulmonary hypertension (PH).
PH patients, families and caregivers around the world have rallied behind the zebra,
building its stripes into their fundraising events, posting photos of themselves in zebra
clothing and talking about the zebra in media interviews about PH. At conferences of
PH-treating professionals, zebra-striped buttons are being given away and participants
are buzzing about “the zebra campaign.”
Why?
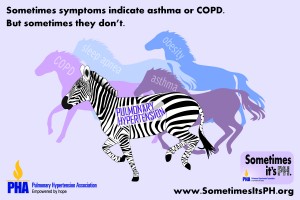
 Among doctors, the zebra is a metaphor for an unexpected diagnosis. That’s why the Pulmonary Hypertension Association (PHA) has made it the symbol of a new 5-year initiative on the importance of considering a PH diagnosis early on. The campaign, Sometimes it’s PH, responds to a major problem — frequent misdiagnosis — by teaching health care professionals to suspect PH, screen for it and team with PH specialists to provide the best possible care.
Among doctors, the zebra is a metaphor for an unexpected diagnosis. That’s why the Pulmonary Hypertension Association (PHA) has made it the symbol of a new 5-year initiative on the importance of considering a PH diagnosis early on. The campaign, Sometimes it’s PH, responds to a major problem — frequent misdiagnosis — by teaching health care professionals to suspect PH, screen for it and team with PH specialists to provide the best possible care.
The zebra image strikes physicians immediately, because it comes straight from
their medical education. When they first learn how to reach a diagnosis, they are
taught, “When you hear hoof beats, think horses, not zebras.” In other words, doctors
learn to assume that common symptoms suggest common diseases. But with a rare
disease like PH, widespread symptoms such as shortness of breath, chest pain, fainting
and fatigue point to a “medical zebra,” similar to a horse, but very different.
Sometimes it’s PH pairs the zebra with this message to medical professionals:
Sometimes shortness of breath, chest pain and other symptoms may lead you to
conclude it’s asthma, COPD, obesity or lack of fitness. But sometimes it’s not.
Sometimes it’s PH.
The campaign aims to eliminate misdiagnosis of this illness, whose symptoms are often mistaken for other diseases. Many patients are misdiagnosed repeatedly over several years. Research shows that almost 75 percent of patients have advanced PH by the time they are diagnosed. That number has scarcely changed since the 1980s. While continuing to work toward a cure, promoting early diagnosis is PHA’s next big priority for improving patient care.
Sometimes it’s PH, led by PH-treating professionals, will educate other professionals
about PH, starting with primary care providers, the first ones patients turn to with symptoms, and later reaching specialists and likely patients. PHA will highlight its own educational programs on early diagnosis; pursue new educational programs outside PHA; communicate through medical journals, media coverage, and more; and it will connect with other groups of medical professionals to carry the early diagnosis message to their members.
Already PHA has highlighted early diagnosis in the summer issue of its medical
journal, Advances in Pulmonary Hypertension; made it the theme of its successful
PH Awareness Month in November; and has offered a webinar for professionals and
patients on the subject during PH Week at the American Thoracic Society. (The journal
and webinar will be archived at www.PHAOnlineUniv.org, PHA’s hub for medical
education, if you’d like to catch it.)
Want to unite with others behind the zebra? Show you endorse the campaign at
www.SometimesitsPH.org. Share your own misdiagnosis stories and zebra photos
there. The site also lets you view a 1-minute video spot and gives tips on sharing it
through social media. Every step strengthens our cause.
Holiday Hours
November 20, 2012In honor of the holiday season, our office will be closed:
December 24th, 25th, 31st and January 1st, 2013.
Thanks and Happy Holidays!
Posted in Featured | Tagged Caring Voice Coalition, CVC | Leave a commentRosemary’s Story
September 21, 2012I was diagnosed with Pulmonary Hypertension November of 2011. The years before that, I was very active. I had earned a Masters Degree in Counseling in 2006, the same year I was diagnosed with asthma. I have since learned that Pulmonary Hypertension is often misdiagnosed as asthma. Despite the diagnosis, I worked full time, took care of my parents, my nephew, and I worked with horses, caring for them and cleaning up after them. I was very physically active, constantly going somewhere or doing something.
Then I started getting tired having more “asthma attacks”. I couldn’t seem to catch my breath. I started sleeping more and becoming less active. I told my doctors that I thought something was wrong with me, but they said, “There is nothing wrong with you. Exercise more, take vitamin D and lose weight”. I knew something more was wrong, but I did what they said.
I forced myself to start doing everything again, despite the exhaustion. I joined a gym and went swimming every single day and changed my diet. I could only eat a yogurt and six crackers twice a day – anything more than that and I would get sick and start coughing badly. I did lose weight but my ankles and legs were swollen from retaining water. I started going to the doctor or ED at least once a month because I couldn’t breathe. I stopped losing weight and started retaining water so badly that I could not put on my shoes.
They said, “It is nothing, just your asthma” and gave me more asthma meds. In July of 2010 the doctor diagnosed me with COPD. I asked to see a specialist, but he refused to refer me, stating the treatments for asthma and COPD were the same. I started having chest pains and my legs were so swollen they were often purple. Again, I was told to lose weight. I no longer had the energy to do anything besides go to work and come home and sleep. I was now going to the ED or my doc 2 to 3 times a month because of the chest pain and shortness of breath, swollen ankles, anxiety attacks, lack of energy and the cough.
I was given a nebulizer and a pat on the head and told to lose weight and get more active. I said “there is something very seriously wrong with me, this is not right”, but no one listened. On Nov 5th, 2011 I was taking a shower and felt a stabbing pain in my right lung – it literally knocked the wind out of me. I could not breathe and it lasted for several seconds. I finally caught my breath, did a nebulizer treatment and went to work. People kept asking if I was alright as I had lost my voice and was coughing every time I moved. I said “it’s just my asthma acting up”. The next day, I went to work and it was a blur – I was in pain, having a hard time catching my breath and then having to stop every few steps to catch my breath. That night I could not sleep because every time I laid back I couldn’t breathe and was coughing constantly.
I went to work the next morning and was only there for three hours before I saw that my fingers had turned purple and again I couldn’t catch my breath. My chest felt like it was on fire and I felt like I was going to die. I told my boss, who told me to go to the hospital or call an ambulance. As soon as I walked in the door of the hospital, the nurse at the check in took one look at me and called out “We need a wheelchair. Shortness of breath”! They took me right back to a room and were undressing me and hooking me up to machines. I was told that I had a blood clot in my right lung and I was being admitted to the hospital.
They sent me to a regular floor, however the nurses there refused me, saying I was to unstable I needed to be an a more acute unit. So, I was sent to the PCU. I told the doctor, Dr. Dexter what had been happening and he said “I don’t think this is just a blood clot, something else is going on”. I asked “Does that mean you are going to discharge me?”, to which he replied, “No, you are not leaving until I know what is wrong with you”. I was on oxygen and hooked up to IV’s, but for the first time in months I was not scared – - someone was finally listening to me. Later, I learned the doctors and nurses were wondering how I was even alive my oxygen was so low. If I had not been talking they would have put a tube down my throat to breathe for me. They said I should have been dead.
Dr. Dexter consulted with Dr. Filner, a pulmonologist before both of them said they felt I had something called Pulmonary Hypertension. Over the course of the next three weeks I was given every test imaginable. Dr. Filner requested a right heart cath, but since it was the day before Thanksgiving the cardiac team did not want to do it. They said it could be done as an outpatient, but thankfully Dr. Filner was insistent. As I was on blood thinners for the blood clot, I had to have a plasma transfusion to slow down my clotting time.
At this time a nurse said I should be discharged since my oxygen level was now at a 100 percent. “I am going to go talk to Dr. Filner about discharging you. We need this bed for really sick people and you can take off that oxygen – you don’t need it”. So I took off the oxygen and watched my numbers drop from 100 percent to 90 percent to 85 percent. The nurse almost immediately returned, very red faced, and put the oxygen back on me saying, “I guess you are staying”. He left and I did not see him again.
Soon thereafter, I had the right heart cath procedure done. At first all the doctors and techs in the room were joking around, talking about what their plans for the holidays were. But then when the surgeon performing the test said “Ok we are in, oh look at this” all of the sudden people got serious and stopped talking. They were asking if I was ok, adjusted my oxygen mask, hooked me up to more wires. The surgeon came around to see my face, laid his hand on my arm and said, “The pressure in your lungs is 80. It is supposed to be four.”
It wasn’t until Dr. Filner came and saw me and told me it was confirmed that I had Pulmonary Hypertension and I would have to quit my job and take meds for the rest of my life. I stopped listening at “quit my job”. I was at the top of my career, I was opening my own office… quit? Never I had worked so hard and long to get were I was. I didn’t hear a word he said as he was explaining things. My boss sent over paperwork for FAMLA which she said would protect my job until I came back. My co-workers took up donations for PTO and money to help my family, as I was out of my own PTO. I was discharged without oxygen and a with a whole lot of new meds.
Three weeks later I went to see Dr. Dexter’s wife, who was considered to be the best when it came to Pulmonary Hypertension. In her office they tested my oxygen levels and she immediately put me back on oxygen. She then told me I would have to be on oxygen 24/7 from now on. I tried going back to work, even though Dr. Dexter said it was not possible, which unfortunately proved to be true. Every time I tried, I was back in the hospital for at least a week. The longest I made it was when my schedule was dropped to 5 hours. I made it for three days but on the fourth, I slept through the day and couldn’t be woken up. I ended up back in the hospital for a month.
That is when I threw in the towel. I told my supervisor who advised me to talk to HR and apply for the life insurance policy. The HR Department took up another collection for me and set up a day for me to quit three days before my FAMLA was up. They did this so that if I ever wanted to work again, it would not reflect poorly on me. The HR Director also helped me with COBRA.
The company raised enough to hold me over until the insurance started, which would match 60 percent of my salary. I was going to receive $1761. It may sound like a lot, but my mortgage and car payment alone took $1000 and COBRA took $531. The oxygen I needed was $50 and the co-pay for doctor’s appointments and meds took up the rest. I had no money for food or gas but thanks to friends and my family, we struggled through.
In August of 2012 I had to choose between making my COBRA payment or getting food for the family. I had already stopped a couple of meds because I could no longer afford them. I was turned down for state assistance because I “made too much money”. I was referred to a helpline and ended up on the phone with Caring Voice. The person who assisted me said that they could help with the COBRA payment, which meant I could now spend that money on food and gas and my other meds that I needed. It was the help I needed at a time when I had lost all hope. I was about to return all the oxygen equipment go off all my meds and drop COBRA. CVC stopped me from having to do that and basically saved my life. ‘Thank you’ just doesn’t seem enough, but it is all I have right now. My gratitude and thanks is all I can give.
Posted in Diseases, Featured, How We Help, Media Center | Tagged Caring Voice Coalition, CVC | 9 CommentsLee Ann’s Story
September 17, 2012It was the third week that my ankles had been swollen consistently. That Wednesday, May 16, 2012 my mother and husband convinced me that an ER trip was necessary. The swelling had come and gone over the past 3 months. As a 41 year old mother of two teenagers, an asthmatic and someone who was overweight, I chalked the swelling up to being heavy. The shortness of breath had been there for years and again, I chalked that up to being heavy. Then I started to notice chest pain with the swelling and shortness of breath. That was when I realized that this might be a little more serious than I thought.
At the ER, the initial thought was that I had had a heart attack. Then blood clots then eventually, the final diagnosis… Pulmonary Hypertension. The language was not new to me or my family as my niece was born two short years ago with PH.
After a whirl of tests and a week-long hospital stay, I was discharged with little knowledge other than what I had learned from my niece. A Cardiac Cath was done and with this I was introduced to my now Pulmonary Doctor whom I love. Now the diagnosis was worse. Pulmonary Hypertension and Pulmonary Veno-Occlusive Disease.
I was told that after 5 years I would have a 50% chance of living without a double lung transplant. My world just stopped. Here we were a family of four making good money and living a great life. I had to quit my job and file for Social Security Disability. I had to deliver the news to my husband and boys that I was going to die.
Here it is four months later; I have had an open lung biopsy and have been taking medications that make my symptoms worse. The money situation is so bad, we’re making enough barely struggle by, but not enough to live. I was approved for disability but have a $5000 out of pocket deductible with my husband’s insurance. Not to mention copays and script costs. Disability wont start until December 26, 2012 and Medicare wont start until May 2014.
Stress is bad, I find myself crying all the time. I try to put on a happy face but it is so hard to ask for help, watch my husband come home tired from work and do housework and cook because I cannot.
Everyone keeps saying it will be ok, my question is ok for who? I have not yet learned to deal with my illness and pray that soon I will see that I can survive.
Thank you Caring Voice Coalition for all you do everyday.
Posted in About Us, Diseases, Events, Featured, How We Help, Media Center | Tagged CVC, Medicare, Pulmonary Hypertension, Pulmonary Veno-Occlusive Disease, Shortness of Breath, Swollen Ankles | 8 Comments ← Previous post