Tag Archives: narcolepsy
Helpful Resources
July 22, 2014Partnerships
Caring Voice Coalition has partnered with LegalShield to offer CVC patients discounted legal plan membership. For a small, flat monthly fee, CVC patients can become LegalShield members, with access to services including unlimited legal advice on any topic, living wills, estate planning, health care proxies, insurance coverage, and identity theft protection. With LegalShield, CVC patients have access to caring, top-quality attorneys from highly-rated law firms across the country at very low cost.
NeedyMeds, founded in 1997, is a non-profit information resource devoted to helping people in need find assistance programs to help them afford their medications and costs related to health care.
Patient Associations
- Alpha-1 Foundation
- Chronic Granulomatous Disease
- Complex Partial Seizures
- Cutaneous Lymphoma
- Factor XIII
- Gaucher’s Disease
- Huntington’s Disease
- Idiopathic Pulmonary Fibrosis
- Infantile Spasms
- Lennox-Gastaut
- Myositis
- Narcolepsy
- Nephrotic Syndrome
- Orthostatic Hypotension
- Pulmonary Hypertension
- Sarcoidosis
- Steven-Johnson Syndrome
- Thalassemia Syndromes
Copayment Assistance Organizations
- The Assistance Fund
- CancerCare
- HealthWell
- Leukemia and Lymphoma Society
- NORD
- Patient Access Network Foundation
- Patient Advocate Foundation
- Patient Services, Inc.
Government Agencies and Programs
- BenefitsCheckUp
- Medicaid
- Medicare
- National Institutes of Health (NIH)
- Social Security Administration
Transplant Information
Posted in How We Help | Tagged Alpha-1 Foundation, BenefitsCheckUp, CancerCare, Chronic Granulomatous Disease, complex partial seizures, Cutaneous Lymphoma, factor XIII, Gaucher’s Disease, HealthWell, Huntington's Disease, idiopathic pulmonary fibrosis, Infantile Spasms, Lennox-Gastaut, Leukemia and Lymphoma Society, Medicaid, Medicare, narcolepsy, National Foundation for Transplants, National Institutes of Health (NIH), NORD, Patient Access Network Foundation, Patient Advocate Foundation, Patient Services Inc, Pulmonary Hypertension, Social Security Administration, Thalassemia Syndromes, The Assistance Fund, United Network for Organ Sharing, UNOS | Leave a commentVideo Testimonials
June 9, 2014
Kindra Cansler, caretaker for her son Justin, an Infantile Spasms patient, tells her story.
Joyce Scannell, a Narcolepsy patient, tells her story.
Beverly McGregor, a Pulmonary Hypertension patient, tells her story.
Supported Diseases
June 9, 2014CVC Disease Funds
Alpha-1 Antitrypsin Deficiency
Chronic Granulomatous Disease
Complex Partial Seizures
Cutaneous Lymphoma
Factor XIII Deficiency
Gaucher’s Disease
Huntington’s Disease
Idiopathic Pulmonary Fibrosis
Infantile Spasms
Inflammatory Eye Disease
Lennox-Gastaut Syndrome
Myositis
Narcolepsy
Nephrotic Syndrome
Orthostatic Hypotension
Pulmonary Hypertension
Sarcoidosis
Severe Chronic Pain
Steven-Johnson Syndrome
Thalassemia Syndromes
Night Vision
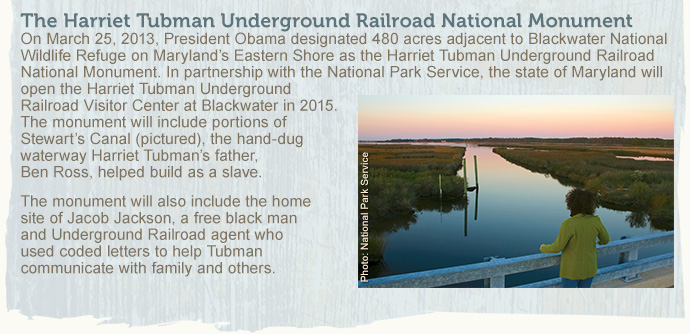
December 10, 2013Community unfolds the remarkable life of the Underground Railroad’s fearless conductor, Harriet Tubman, who suffered during much of her life from a chronic, debilitating disorder. Eva Leonard reports.
 Araminta Ross, who later become known as Harriet Tubman, “the Conductor of the Underground Railroad,” “General Tubman,” and “Moses,” was born to Benjamin Ross and Harriet Green, one of nine children, sometime between 1820 and 1824 in Dorchester County, Maryland, on the plantation of Anthony Thompson.
Araminta Ross, who later become known as Harriet Tubman, “the Conductor of the Underground Railroad,” “General Tubman,” and “Moses,” was born to Benjamin Ross and Harriet Green, one of nine children, sometime between 1820 and 1824 in Dorchester County, Maryland, on the plantation of Anthony Thompson.
Tubman’s birth year is uncertain, however a record of a payment to a midwife indicates that it was probably 1822. As an adult, she took her mother’s name, “Harriet,” and the surname, “Tubman,” when she married John Tubman.
Tubman’s father was enslaved by Thompson, while she, her mother, and her siblings were enslaved by Thompson’s stepson, the farmer Edward Brodess. As a very young child, Araminta, who was known as “Minty,” was put to work. Brodess hired her out to other landowners, who treated her cruelly, brutally whipping her, and leaving deep scars. Even when sick with measles, Tubman was forced to haul muskrat traps through frozen swamps, wearing no shoes, her feet only covered with cloth.
As a teenager, following a severe head injury—the result of her efforts to protect another slave—Tubman developed a lifelong, chronic condition, with debilitating symptoms that have been described as being similar to those of narcolepsy and temporal lobe epilepsy.
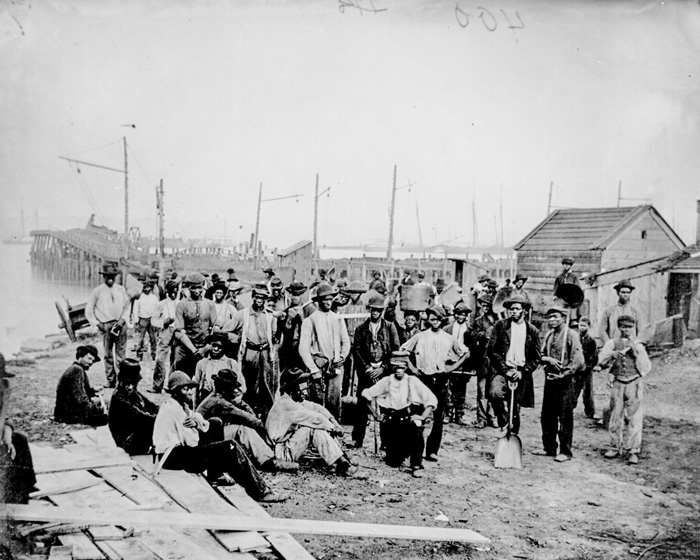
(Above) Freedmen laborers at Quartermaster’s Wharf, Alexandria, Virginia. African-American dockworkers and mariners taught Harriet Tubman to follow the North Star to freedom. Photo: Mathew Brady, U.S. National Archives and Records Administration (Below, right) A two-pound counterweight of the type that fractured Tubman’s skull, causing her life-long disability. Photo: Eva Leonard
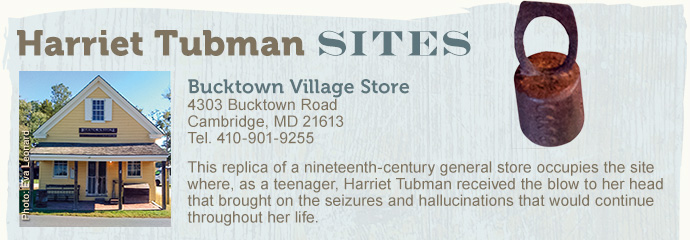

At the local general store, she had encountered an unidentified young male slave, there without permission. An overseer ordered Tubman to restrain the young man, and hurled a two-pound counterweight at him. Instead, after he darted out of the store, Tubman blocked the doorway. The weight hit Tubman in the head, fracturing her skull and nearly killing her.
Recovering from the blow without medical care, she was forced back to work only two days later, as her head bled from the injury. After the injury, Tubman began to experience uncontrollable episodes, which could happen several times a day, as she fell into a motionless, dream-like state, lasting from half an hour to an hour, during which she hallucinated.
The attacks occurred without warning, even in the middle of conversation. When an attack ended, she resumed the conversation where it had stopped. Tubman described the hallucinations as “visions,” in which she sometimes saw herself flying above the earth and over water.
Kate Larson, author of “Harriet Tubman, Portrait of An American Hero: Bound for the Promised Land,” says that during these states, Tubman also heard the sounds of voices, screams, music, and rushing water, and felt as though her skin was on fire, while still conscious and aware of what was going on around her. She also experienced extreme, debilitating headaches, and became increasingly religious after the injury.
Initially, Tubman’s injuries made it difficult for her to work and lowered her value as a slave, and she was returned to Brodess. But she grew stronger as she recovered and worked digging out stumps, plowing fields, chopping wood, and hauling timber.
In 1844, at the age of 25, she married John Tubman, a free black man. When Edward Brodess died in March of 1849, he left his wife, Eliza, deeply in debt. Fearful that Eliza Brodess would further split up her family by selling them South to work on chain gangs to pay the debt, Tubman escaped to Philadelphia later that year. (She had watched her two older sisters, Linah and Soph, sold out of state as part of a chain gang when she was younger.)
She traveled the approximately 90 miles to Philadelphia on foot, at night, following the North Star, which she had learned of from the African-American dockworkers and mariners she befriended as she loaded and unloaded produce at the wharves. The mariners served as a vital link in the Underground Railroad’s communication network, delivering coded messages and providing information about the outside world for those seeking freedom.
On her way to Philadelphia, Tubman stopped at Underground Railroad safe houses, where she was fed, sheltered and directed to the next house by Quakers and black and white abolitionists.
Tubman described her emotions on finally crossing the border into the free state of Pennsylvania: “I had crossed the line of which I had so long been dreaming. I was free, but there was no one to welcome me to the land of freedom. I was a stranger in a strange land, and my home after all was down in the old cabin quarter, with the old folks, and my brothers and sisters. But to this solemn resolution I came; I was free, and they should be free also; I would make a home for them in the North and the Lord helping me, I would bring them all there.”
In Philadelphia, and in Cape May, New Jersey, Tubman found work as a domestic, and as a cook in hotels, earning money to return to Maryland and bring her family to freedom.
In 1850, Tubman made her first trip back to Maryland to retrieve her niece and her niece’s son and daughter. In 1851, she came back for her husband, John Tubman, but discovered that he had remarried and did not want to join her. Instead, she found a group of slaves eager to leave, and brought them to Pennsylvania with her.
During an estimated 13 trips, over the course of a decade, Tubman brought at least 70 slaves, including many family members, to freedom, never losing a passenger. Following the passage of the Fugitive Slave Act of 1850, it was no longer safe to end the journey in the northern states, so Tubman began to bring her passengers to Saint Catharines, Ontario, Canada, where she moved in 1851.
In 1854, Tubman sent a coded letter through a friend to Jacob Jackson, a free, literate black man who lived near Tubman’s family in Maryland. The letter alerted Tubman’s three brothers to her plans to return and bring them back with her to Philadelphia. In 1857, she also brought her elderly parents to freedom.
Tubman led her escapes at night, following the North Star, using a variety of strategies to evade detection and capture. On one trip she disguised herself as a man, and on another, she carried chickens to make it look as though she were running errands. She sometimes wore a silk dress to appear a free, middle-class woman, and she often led Saturday night departures because “Wanted” posters could not be printed until Monday mornings, giving her a one-day head start.
Tubman carried the drug paregoric to prevent babies from crying during the trip. She also packed a pistol as protection against slave catchers, and as a warning for passengers who might be tempted to abandon the escape and turn back. Tubman was fearful that if they did turn back, they would divulge what they knew about the Underground Railroad.
In a December 29, 1854 letter, Thomas Garret, Wilmington, Delaware Underground Railroad Stationmaster wrote to J. Miller McKim: “We made arrangements last night, and sent away Harriet Tubman, with six men and one woman to Allen Agnew’s, to be forwarded across the country to the city. Harriet, and one of the men had worn the shoes off their feet, and I gave them two dollars to help fit them out, and directed a carriage to be hired at my expense, to take them out….”
 In 1859, Tubman moved to Auburn, New York, purchasing a house from her friend, Senator William H. Seward, and bringing her parents with her. She would also open her home to other relatives, as well as friends and former slaves.
In 1859, Tubman moved to Auburn, New York, purchasing a house from her friend, Senator William H. Seward, and bringing her parents with her. She would also open her home to other relatives, as well as friends and former slaves.
After the Civil War began in 1861, Tubman worked with the Union Army in South Carolina, Virginia, and Florida as a scout, spy, leader, and nurse. Known for her abilities as a healer and a caregiver, Tubman brought ill soldiers back to health, using herbal treatments she knew from growing up in the Maryland countryside, and drugs she had learned about from Edward Brodess’s stepbrother, a doctor who ran a pharmacy. To heal soldiers who were sick, and in some cases, dying, from dysentery, she treated them with a tea she brewed using herbs and roots with medicinal properties.
Disguising herself as a sick, elderly woman, she performed reconnaissance for the Union army in Confederate towns. In 1863 Tubman scouted and planned for the Raid at Combahee Ferry, commanded by Colonel James Montgomery, and led 300 black soldiers during the raid, which freed more than 700 slaves in South Carolina. Tubman also recruited volunteers for John Brown’s raid on Harpers Ferry, West Virginia, but was unable to join the raid.
In 1869, Tubman married Union Army veteran Nelson Davis, whom she had met in Auburn. Despite her own accomplishments, Tubman was for many years denied her own military pension, although she received one as Davis’ widow after he died. She finally was granted one for her own service in 1899.
Sometime during the late 1890s, Tubman had brain surgery at Boston’s Massachusetts General Hospital to relieve the pain she had dealt with much of her life from her childhood injury. Although details are scarce, the operation gave her some relief from the symptoms caused by the blow she had received some 60 years earlier.
In 1908, Tubman founded the Harriet Tubman Home for the Aged in Auburn, New York. Her friend and neighbor Helen Tatlock said that at her home, Tubman took care of “the demented, the epileptic, the blind, the paralyzed, [and] the consumptive.” When Tubman herself grew frail, she would be cared for in the home she had established.
When Harriet Tubman died of pneumonia in 1913 in Auburn, New York, she was buried with full military honors at Fort Hill Cemetery. Nearly fifty years earlier, the abolitionist Frederick Douglass, had written in a letter to Tubman: “The difference between us is very marked. Most that I have done and suffered in the service of our cause has been in public, and I have received much encouragement at every step of the way. You, on the other hand, have labored in a private way. I have wrought in the day—you in the night. … The midnight sky and the silent stars have been the witnesses of your devotion to freedom and of your heroism.”
Posted in About Us, Diseases, Featured | Tagged anthony thompson, araminta ross, benjamin ross, blind, bucktown village store, chronic disease, combahee ferry, disorder, edward brodess, Epilepsy, fort hill cemetery, frederick douglass, harriet green, harriet tubman, harriet tubman home for the aged, harriet tubman museum and educational center, harriet tubman underground railroad national monument, helen tatlock, hunting creek, j. miller mckim, jacob jackson, james montgomery, john tubman, johnson house, kate larson, narcolepsy, nelson davis, neurological disorder, paralyzed, pneumonia, poplar neck, portrait of an american hero, temporal lobe epilepsy, thomas garret, underground railroad, william seward | 9 CommentsIn Your Words: Elaine Kelley
September 27, 2013Sixteen-year-old Elaine Kelley’s narcolepsy symptoms first appeared in July 2011, shortly before she started her freshman year of high school in Tulsa, Oklahoma.
“The first thing I noticed was the cataplexy,” she recalls. “It came on very suddenly. Laughing would make me very weak, and I thought that was strange. Then it just progressively got worse.
“I told my mom about it. Then I also started sleeping a lot during the day. We thought that was strange too.”

From from left to right: Elaine Kelley's mother, Vickie Kelley; brother, Joe Kelley; father, Marshall Kelley; and Elaine.
The cataplexy attacks first occurred at home and at her cousin’s house. Then, Elaine says, “It happened big time when we were shopping for school shoes, and I was yelling for my mom, asking her to come look.” Fortunately, Elaine wasn’t hurt when she collapsed in the shoe store, but she says, “That’s when we knew it was serious.
“One night I had a cataplexy attack, and my dad saw it for the first time. He wanted to take me to the hospital. We were just going to go to an urgent care center, but it was closed.
“The next day, we called my pediatrician, and she wanted me to check into the hospital. I checked in the next day and went through a 24-hour EKG and an EEG and spent the night there. They couldn’t find anything. They had a recording of me having cataplexy and still couldn’t figure it out, because they had never seen it before.
“They thought it was epilepsy, anemia, or something neurological, but everything came back normal. They might have said that it could be narcolepsy, but they never said ‘cataplexy.’
Elaine explains how she ended up essentially diagnosing herself. “I started googling ‘laughing and falling,’ and that’s when I came across cataplexy. So I looked into that because there was a story about a lady who had it.
“We called my pediatrician; she referred us to a sleep specialist, and I took the sleep test. I was lucky to figure it out pretty quickly, after a few months of the symptoms, because school had started.
Elaine did have cataplexy episodes at school, but luckily, she was in the bathroom with friends when they occurred. “All my friends knew about it and were supportive, which was nice,” she recalls.
She describes her initial attempts to prevent the cataplexy on her own. “It took a lot of self-control to try to not let it happen. I would clench my fists really tight if I felt it coming on and tighten my body so I wouldn’t lose muscle control. I noticed that it did help a little.
“But once I got the right medication and figured all that out, the cataplexy has never gone back to the way it was when it was at its worst.
“I still have daytime sleepiness, but a 30-minute nap once a day helps that. I still notice that when I laugh, sometimes I lose control of my facial muscles a little bit.
“I’m very lucky. I have a strong support system with my friends and family. I play soccer. I like to babysit. I like spending time with my friends.
“I want to go to college. I really love history, so I want to major in that. My reach school is Brown; that’s what I’m shooting for. If not, I’ll probably go to the University of Oklahoma or the University of Kansas—somewhere close to home.

From left to right: Elaine Kelley; brother, Joe; and mother, Vickie.
“When I first was diagnosed, my dad sent out an email letting all my teachers know. They were all really curious. There was actually another kid who graduated last year who had narcolepsy, and I was able to talk to him about it.
“People ask me about it a lot. I have no problems explaining it.
There was a rumor at school that when I get excited, I fall asleep. That’s what some kids twisted cataplexy into. I set everyone straight.
Elaine says there are a couple of things she’d like people to know about narcolepsy: “I’d like to make it clear that I don’t fall asleep standing up, because a lot of people ask me that.”
She also says that if there’s one thing she’d like people to be aware of, it’s to be thankful to have a sleep cycle. “Because I sure do miss that.”
For those teens and children who’ve been diagnosed with narcolepsy, she adds, “Don’t be ashamed or embarrassed that you have it. I struggled with that. But if you’re confident about it, it makes it a lot easier.” —EL
Posted in About Us, Diseases, Featured | Tagged anemia, Cataplexy, cataplexy attack, ECG, EEG, EKG, Elaine Kelley, electrocardiogram, Electroencephalography, Epilepsy, in your words, laughing and falling, narcolepsy, neurological disorder, patient profile, sleep, sleep specialist, sleep study, sleep test | 5 CommentsDonate Now
August 20, 2013Give Financially
Caring Voice Coalition has established a safe, secure way for you to make an on-line donation. By donating to Caring Voice Coalition, you are making a difference in the life of a patient. Caring Voice Coalition and our donors have a common goal – to help as many patients as possible. The Caring Voice Coalition is a qualified 501(c)(3) tax-exempt organization and donations are tax-deductible to the full extent of the law. Our Federal EIN is 26-0058446.
Please fill out this form and click submit to be taken to our secure payment feature where you’ll be able to make a donation with a debit or credit card.
If you prefer to send your donation by mail, please send your check made payable to Caring Voice Coalition to:
Caring Voice Coalition
8249 Meadowbridge Road
Mechanicsville, VA 23116
Thank you for your generous commitment of funds. Every dollar makes a difference!
Seeking Support
November 28, 2012Whether you’re newly diagnosed with a condition, or have been living with it for years, getting the support you need is crucial to maintaining your best healthy life, both physically and mentally. There are tons of ways to participate in support groups, whether it be through an actual physical get-together, online meetings, or even actively participating in message boards.
The benefits of support groups are obvious – being in an environment in which other people understand you and can share helpful advice and motivation is always going to be an aid, however it’s important to see how this engagement can benefit your personal relationships. It can be truly difficult for someone to give the support they want to a person with a chronic illness, because they don’t truly understand or know what to say. And it can be equally hard for the person affected to really share in words what is going on in their minds and with their bodies. Going to an outside source of support can create a better bond between the caregiver and the person who is ill.
Often times, people are hesitant to go to support groups because they feel what they are going through is too personal or intimate to share with a room full of strangers. So, if you’re feeling hesitant, think about the benefits of just going and listening. It can be more beneficial than you may believe to just be silent for an hour and soak up what others are saying. And if going to a support session seems like you are relinquishing some of your independence, just remember that everyone needs a helping hand sometimes, just don’t be afraid to take it.
Below are some great resources for support groups from some of our friends in the rare and chronic disease community. Also, don’t hesitate to ask your doctor or medical professional where to look.
Pulmonary Hypertension Association
Pulmonary Hypertension Central
MD Junction Pulmonary Hypertension Online Support Group
Daily Strength Pulmonary Hypertension Online Support Group
Pulmonary Hypertension South Africa
Pulmonary Fibrosis Foundation
Daily Strength Pulmonary Fibrosis Support
Coalition for Pulmonary Fibrosis
MD Junction Pulmonary Fibrosis Online Support Group
Narcolepsy Network
Daily Strength Narcolepsy Online Support Groups
Narcolepsy Online Support Groups
Huntington’s Disease Society of America
Daily Strength Huntington’s Disease Online Support Groups
Huntington’s Disease Lighthouse Families Online Support Groups
Huntington’s Disease Advocacy Center Message Boards
Huntington’s Disease Youth Organization
Infantile Spasms Center
The Infantile Spasms Community Board
Alpha-1 Association
Daily Strength Alpha-1 Online Support Groups
Are there support groups which you have found helpful? Please share with us!
Posted in Caregivers, Diseases, Featured, Media Center, Uncategorized | Tagged chronic illness, Infantile Spasms, narcolepsy, Pulmonary Fibrosis, Pulmonary Hypertension, Support, Support Groups | 3 CommentsJulie Ann’s Story
July 6, 2012Twenty-five years. I keep repeating that over and over again. It’s taken nearly twenty-five years for me to get the answers I’ve been seeking about what is happening to my body and what is wrong with me. Talk about a long road!
Nobody in my family is sure exactly when it all started anymore. The first “episode” that I can clearly recall happened during the National Anthem while I was in my kindergarten classroom. I was five years old. I remember not knowing what the strange feeling was in my head or my body. I remember hearing everyone around me talking, but suddenly not being able to see, move, or speak, and not knowing what exactly was going on. The Anthem was still playing. The teacher was calling my name, asking me to wake up. I was awake! Why can’t I talk?! Why can’t I move?! Why can’t I open my eyes?! I was terrified that I was dying. Finally, and suddenly, I could open my eyes, and squeak out a sound. Then, I could move a little. I wasn’t sure what was going on, but I was terrified. And thus began a nearly twenty-five year journey full of doctors, tests, misdiagnoses, medications, hospital visits, and searching for the answers.
From that point on, episodes similar to that one continued to occur again and again. They happened at school, at home, at friends’ or neighbors’ homes, in public places, and at various places where I’ve worked. Doctors gave me a plethora of diagnoses– hypoglycemia, vasovagal syncope, seizure disorders, panic disorders, just to name a few– and treated me for those disorders, but the episodes kept happening. Even when I wouldn’t have complete collapses, there were innumerable occasions when I’d feel just the same as I do before my body gives out. It starts with an odd tingling sensation in my head. The next warning is a tunneling of my vision, where I can only see in a narrow stream in front of me. Shortly thereafter, my body is overcome with a weakness and a sensation I can only describe as an odd numbness. Often times, this is where things stay for a bit. These occasions happen anywhere from once daily to over twenty times in a day. On the occasions when my body collapses, I stay awake, but fully paralyzed. I can’t feel, see, move, or speak, no matter how hard I try. I am aware, I can hear and understand sounds and voices, but that’s all. I’ve described this repeatedly for nearly twenty-five years. No one could help me.
Last year, I complained to my then-current primary care physician about these “episodes” that don’t result in full collapse, not even thinking that they might be related to the collapses. I’d had several collapses, as well, in the midst of these complaints and issues, so she sent me around to each of my current specialists to have them look me over. After the cardiologist, endocrinologist, and neurologist all sent back unremarkable reports, she called me back into her office. I again explained my complaint to her, and again explained that I had been battling severe exhaustion, fatigue, and sleepiness– to the point where I was yawning incessantly all day every day, regardless of how much I slept the night before–and how these issues have been getting progressively worse, regardless of my attempts at correcting them by eliminating caffeine, resting more, watching my diet, losing a LOT of weight (on purpose), and other suggested lifestyle changes.
The statement about the incessant yawning became the turning point in my medical history. When the doctor suggested that I might have narcolepsy, I thought she was a bit crazy. I left the office with the referral and figured one more appointment wouldn’t be so bad. After a brief appointment containing a ton of seemingly random and unrelated questions with the sleep medicine specialist, he said he agreed with my PCP on her narcolepsy theory. He wrote me a prescription for a narcolepsy medication, gave me a list of topics related to narcolepsy to research, and scheduled me for a sleep study.
The medication improved my daytime sleepiness immediately and incredibly. The research I did at his suggestion showed so many similarities to my own issues that it felt as if these articles had been written about me. The sleep study confirmed his diagnosis both because of the monitoring results and because of the fact that I had one of these full-body collapse episodes while there at the lab, unfortunately bruising my face up badly. Thankfully, however, the episode was caught on the video monitoring system, and he was able to see what happened and tell me what it was.
It’s called cataplexy, and it’s a symptom nearly exclusive to narcolepsy. When Dr. Winter came to my room just shortly after it happened to check on me, he said something that I will never forget:
“It’s cataplexy, and we’re going to fix it.”
There it was– the name for what was happening to my body for all these years, and a doctor who said it could be fixed! The next morning, November 22nd, 2011, I sat in his office and, for the first time, got to see myself collapsing. I watched, silent and heartbroken, as the video played. I was sickened to think that this is what my family and friends had been seeing for so many years. I’ve been told so many things, by so many doctors. Some had even told me it was all in my head! I refused to stop looking for an answer. I knew that someday I’d find that one puzzle piece that made everything fit. That day was November 22, 2011. That piece is narcolepsy with cataplexy.
Getting my diagnosis, and my answer, is freeing, and at the same time very constricting. There is nothing available today that is going to cure me. Even with multiple medications, I’ll still have to deal with this for the rest of my life. But I know what I’m up against. Scheduling medications, scheduling sleep, wake-up, naps… It’s all a balance. But I’ll figure it out as I go.
It took me almost twenty-five years to get here. It’s time to start the next leg of this journey. So what is next?
Treatment. Medications and lifestyle changes are important to help cope with and manage the symptoms and complications of narcolepsy with cataplexy. It’s going to be frustrating, and it’ll take some time for me to adjust, but it will be well worth the effort. Trying out different stimulants to find something that might work well enough to keep me awake during the day so that I can accomplish the things I want out of life will be tricky, and will come with disappointments along the way. I’ve already had to switch to a different stimulant because the first stopped working, and even on the newer one twice daily, I constantly feel sleepy and exhausted. The options available for treating narcolepsy aren’t foolproof, and they’ll never make me have the energy of someone who doesn’t have the condition. Nothing will. I need to learn to accept that, and so do my friends and loved ones.
Education. Very few people know anything at all about narcolepsy, and even fewer know about cataplexy. Affected people go an average of 10-15 years between the onset of symptoms and a proper diagnosis. I am joining the push for more awareness and understanding of this potentially debilitating illness.
After twenty-five years, I can finally take the first step. And I’m ready to take it. Thanks to Caring Voice Coalition, I can afford to take the steps toward doing what I need to do, so that I can achieve the things I want in my life. My case manager, Lauren, is the absolute most amazing person to work with on everything related to my medications, insurance, etc. I can’t begin to thank CVC, or Lauren, enough.
Posted in Diseases, Featured, Media Center | Tagged Cataplexy, julie ann, Misdiagnosis, narcolepsy, Share Your Story | 3 CommentsShadow Dancer
May 16, 2012By Alex Withrow
The first question I like to ask anyone who makes a living doing what they love, is how they initially became inspired by their profession. And in the time I spent getting to know Trinity Hamilton (in our e-mail exchanges and phone conversations, and my subsequent research of her, her work, and her disease), her answer to that question is by far the most profound thing she said to me. But more on that later.
THE DREAM
Trinity Hamilton became a dancer by mistake. Or, more accurately, by coincidence.

When she was four, her dancing in front of babysitters and family members led her mother to enroll her in a ballet studio. By nine, it was an ongoing joke within the family that Trinity was going to skip college and be a professional ballerina. By 16, she was dancing six days a week and competing regularly.
“From that very early age, I was fascinated by dance,” Trinity said. “I never wanted to be a cheerleader, or hang out with friends after school – it was all about the dancing.”
By her senior year of high school, Trinity had a contract to attend BalletMet in Columbus, Ohio, which she ultimately turned down as the result of a debilitating back injury. A few years later, she was a dancer with Joffrey Ballet in Chicago, which the New York Times has described as one of the top three ballet companies in America.
Joffrey was everything she had hoped. She was “eating, sleeping, and living dance,” carrying out the dream that she had set for herself as a young girl. But in 2000, her childhood bouts of exhaustion (which she and her family had always written off as fatigue from dancing and going to school full time) were catching up with her. Whenever the dancers were given a short break, you could often find Trinity asleep in a corner somewhere. She began falling asleep on the train to work and on the train going back home, often waking up in seedy areas of Chicago. She began to speak lucidly, unaware of what she was saying, and hallucinating regularly. Finally, her ballet master suggested she see a doctor, and when she was 20 years old, Trinity was diagnosed with narcolepsy.
THE DISEASE
“The specialists I work with and I actually don’t know when I started getting narcoleptic symptoms,” she said. “Because looking back, my parents and I realize that sleeping had been an ongoing struggle of mine for quite some time.”
The medication Trinity was prescribed “helped her get through the day,” but two years later, she started feeling symptoms of cataplexy, an affliction often associated with narcolepsy, in which patients suffer chance bouts of muscle loss and/or weakness. These attacks, while usually brought on by strong emotions, occur at random and have proven to be fatal.
“I didn’t even know what cataplexy was,” Trinity said. “I was diagnosed, and soon prescribed medication. It helped, but I was always so afraid of falling on stage. And with that fear came doubt and lack of confidence. That’s when things started to get really bad for me.”
THE DOWNFALL
In the years after being diagnosed with cataplexy, Trinity said she began losing everything – confidence, the ability to stay awake during rehearsals, control over her limbs and movements – everything.
In 2004, she left the stage and moved to Florida to be closer to her parents. She attempted to remain active within the dancing community, teaching and choreographing at schools, and even acting as the ballet director and resident choreographer for the New Tampa Dance Theater. But when she was alone, a perfect storm of pity, self doubt and regret boiled inside her. She gained weight, left the house less and less, and became stuck in her own depression.
“I was at the lowest of my lows,” she said. “I remember looking in the mirror and not seeing a dancer anymore. I had no idea what I was doing with my future. It was a very scary time for me.” In the midst of her depression, Trinity crossed paths with a “phenomenal and remarkably patient” individual named Dr. Neil Feldman, who currently serves as the Medical Director of the St. Petersburg Sleep Disorders Center in St. Petersburg, Florida.
Dr. Feldman understood. He listened. He offered Trinity medical advice in the form of a medication prescribed for narcolepsy. Trinity was opposed to the idea of going on the medication. She feared the lifestyle change, and the drug’s potential side effects. After years of patiently attempting to convince Trinity that it was her best option, Feldman set up an interview between Trinity and one of his patients who was taking the medication. That helped. “A few days later, I began taking it,” she said. “And everything started changing. Everything.”
THE RESURRECTION
Finding a suitable dosage and getting used to the side effects of the drug proved to be a difficult process for Trinity, but once she found the right balance, everything began to fall into place.
After the first month, she was not only staying awake throughout the day, but remaining alert as well. She could drive, she could think – she felt productive for the first time in years. During the second month, the symptoms for cataplexy became dormant.
“Slowly but surely, I began feeling normal again,” she said. “And that’s when I realized I needed to get into shape. I was given a second chance, and I had to give it another try.”
It’s a long road from your self-described lowest low to a stage on the Las Vegas strip, and it didn’t come easy. Hamilton put herself through a “Biggest Loser-style boot camp,” practicing hot yoga regularly, hiring a personal trainer, shedding pounds; whatever it took to gently ease her point shoes back on. By the summer of 2008, nearly a year after starting the drug, she was back to her “fighting weight.”
She attended a professional workshop in San Francisco with Lines Ballet Company, and it was there that Trinity was given the big push she needed.
“The artistic director of Lines was a former colleague of mine at Joffrey,” she said. “And he kept encouraging me to stop teaching and get back on stage. That was a big jump for me, having other professional dancers telling me that I needed to be performing.”
After auditioning for a few companies, she packed up and prepared to move to L.A. Days before she was set to move, she received a call from Cirque du Soleil asking her to come audition for Mystère in Las Vegas. She flew to Vegas and auditioned on Halloween day, 2009. In mid-November, Cirque called back with their offer. A month later, Trinity was living in Las Vegas as a working dancer with Cirque du Soleil.
“It’s funny,” she said. “Attending Joffrey was my childhood dream, and once I started getting back into shape, Cirque du Soleil was everything I wanted for myself. It was one of those amazing dream come true situations. Again.”
THE LIFE
Here’s how a day in the life of a Mystère dancer typically works: You arrive at the Treasure Island theater by 4 p.m., rehearse, do a show (or two), leave at 11:30 p.m., home by midnight, wind down, go to sleep. You’re off Thursdays and Fridays, two weeks in January, a week in May and a week in September. You work every holiday, totaling roughly 475 shows a year.
Trinity’s first year in Vegas was tough. She didn’t know anyone, and was getting used to the town and the lifestyle, adjusting to a new sleep schedule, and so on. It was all work for her.
“It was important to make sure I could live up to the challenge,” she said. “So for that first year, I was firing on all cylinders. I had to make it through that first year with no problems.”
The hard work paid off. Her dancing was strong, her confidence was newly fulfilled; she was back to living her dream.
THE MOTIVATION
Today, Trinity has made a life for herself in what she describes as a beautiful town. “Vegas has this persona of being… Sin City,” she says with a laugh. “But outside of that, it really is a lovely town, a sprawling suburbia off the Strip. It’s actually a very normal life.”
When I ask her if her sleep is okay, she eases out a, “Yeah,” with an audible sigh of relief. “I have to make a point to sleep,” she says. “So sometimes I miss out on things. It’s Vegas, so there is something to do at every hour. But birthday parties, or get-togethers after shows, I usually have to skip out on those. Sometimes I’m asked to volunteer for PR gigs with Cirque, which I’d love to do, but because they are early in the morning, I just can’t. Medically, I can’t. It’s a little tough, missing out on those social engagements, but I have to get eight hours of sleep.”
When I broach the issue of how narcolepsy is often depicted with humor in pop culture, Trinity’s tone becomes serious.
“It is an extremely misunderstood disease,” she says. “In terms of how it is depicted, it’s just a matter of getting people educated. People think that narcolepsy is uncommon, and I know it is considered a rare disease, but statistically, it’s as common as Lou Gehrig’s and MS, I believe.” (According to the National Library of Medicine, approximately 15,500 Americans live with Lou Gehrig’s disease, 155,500 have narcolepsy, and roughly 300,000 people suffer from multiple sclerosis.)
“You bring up narcolepsy, and people know it as that falling-asleep disease,” she says. ”But there’s a seriousness about it that people should be aware of. The more education there is about it, the closer we may be to finding a cure.”
When asked if she has any advice for people who are afraid to fight for their dreams, Trinity’s response is optimistically direct.
“Everyone has challenges in their life,” she says. “Even in the darkest of times, I reminded myself that I had to value and appreciate what I had. I honestly do not know what inspired me to become a dancer. That remains one of those beautiful mysteries. But I’ve always been inspired by other amazing stories. By people who have fought in wars, or have other diseases, or stay at home and raise their children. We all have our challenges, but in terms of living out our dreams, of taking that leap, the biggest fear is within ourselves.”
It’s interesting that Trinity gains inspiration from other amazing stories. Call it a hunch, but it wouldn’t be surprising if hers inspires a few people as well.
Posted in Diseases, Featured, Media Center, Uncategorized | Tagged Ballerina, blog, Caring Voice Community, Cataplexy, CVC, narcolepsy, Trinity Hamilton | 3 CommentsThe Day Started Off Normal Enough
March 14, 2012You awoke to the sounds of the alarm, the radio, the smell of coffee, and the buzzing of your phone. You use everything available to wake up in the morning. You can’t afford to lose another job because you’ve overslept.
You’re still rushing to get ready, and the cold-shower-trick doesn’t wake you as much as it leaves you shivering and cranky. You can live with some shampoo in your hair.
_____________________________________
You head to court. It’s not your normal routine, but you need to take care of that ticket. You were only at the light for a moment. It had been a hard day at work, and the heat had just really started cranking on such a cold day. It’s not like you had RUN a traffic light. You were at a complete stop. The officer who happened to be sitting behind you just really didn’t understand how you could have zoned out in such a short amount of time. The sobriety test was humiliating enough without the ticket.
______________________________________
The good news is that you were able to barter down your traffic “violation” with a promise of driving school. The bad news is that you’re going to have to pay the contempt of court fine. The bailiff shouldn’t have been so forceful when he woke you. It’s really his own fault that you hit him. You’re easily startled.
______________________________________
You made it through work. That proposal had to be rewritten, but you made the deadline. It seemed fine yesterday, but how did you miss so many typos? Oh, well. Done now, and on to a glass of cabernet. Must remember to be careful with the santuko. The garlic needs to be paper-thin, but that knife is sharp. Another trip for stitches is the last thing that you need today. A sizzle tells you that the olive oil in the sauté pan is just about ready…
…At least the fireman was cute.
______________________________________
Not really so funny, is it? And not really so rare, either. Narcolepsy in some form affects about 1 in 2,000 people. Many go undiagnosed. Most see the first symptoms in their teens, but that isn’t a hard rule. Two of the most common symptoms are excessive sleepiness and a loss of muscle control (or cataplexy), but others may experience hallucinations, sleepwalking, or any of a host of other sleep-related symptoms.
As you can see, having narcolepsy comes with a set of inherent dangers, and there is no cure. There are a variety of treatments and medications that can help, but there are some things that you can do right away to help lead a normal life.
Your first step is to seek a diagnosis. If you think that you have a sleep disorder, try taking the Epworth Sleepiness Scale Test. While it is not a professional diagnosis, it is a valuable tool to help determine whether or not to seek a doctor’s advice. Kind of like a high fever and sore throat. Check and check; time for some antibiotics.
Step two is evaluating your lifestyle. Is your addiction to diet soda impacting your ability sleep properly? Caffeine, alcohol, and nicotine have all been shown to interfere with sleep. So have many over-the-counter medications. While it may be inconvenient and you may miss the taste, your diet can play an important part in managing your sleep.
Step three is documenting your life. If you need to work on a large project, try to break it up into smaller, more manageable pieces. Become a note-taker. Not only will it help you to track your progress, it can become a great tool for managing your narcolepsy. You may find that certain foods, situations, or activities trigger a rash of symptoms. You’ll now have a journal that you can share with your doctor, and a reminder of what to avoid.
While certainly not the final step, the last we will impart for today is to SHARE! Your coworkers can help you to stay caught up at work. Your fellow students will surely share some lecture notes. Sharing with others makes having narcolepsy a part of who you are, like having blonde hair or being left-handed, and less of a parlor trick. If things work out with the fireman, he should be willing to drive. And who knows, he may be pretty handy with a Japanese chef’s knife.
Posted in Diseases, Featured, Media Center | Tagged narcolepsy | 1 Comment
What’s Your Story?
February 7, 2012We’ve been thrilled with the reaction to our website, and we really enjoy sharing with our many fans on Facebook. We get to share with you tips for healthy living, breaking news about medical research, and stories of hope and courage.
It is the stories of the people that we’ve helped that have inspired us the most.
We shared the story of Justin, and how his mother has struggled to raise him. Kindra is like many other moms, married and raising children, but her story has a twist: In addition to school, groceries, and family, she seeks answers for dealing with Justin’s pachygyria and infantile spasms. Her story touched us, and led us to the story of Marissa and her father’s chronicle of her life.
We got to tell you about Meghan. She was 2 when her father was diagnosed with Huntington’s disease. As she started college and began to plan her own adult life, she also received a diagnosis of the disease. Her father’s illness gave her a 50/50 chance of having it herself, and the coin flipped against her. Meghan didn’t give up, though. She graduated college and is sharing her story on YouTube and is hosting a concert to spread awareness of her disease.
Roberta has a story like many of the people that we talk to. She went through months of illness, testing, misdiagnosis, and was finally told that she had Pulmonary Fibrosis. After reaching several roadblocks in her journey to treatment, she made a right turn and found us on her road. She still has many hills to cross, but breathes easier knowing that she has an advocate in Caring Voice Coalition.
Matthew went from an active lifestyle to one of uncertainty after a diagnosis of Alpha 1. Many people commented on his story. They shared with us their own tales of fear and uncertainty, and of the struggles that they had endured in a quest for treatment. Matthew’s stories put us back in touch with Steven, whose mother died of Alpha 1. We became involved with Steven after his own diagnosis, and it was wonderful to help him, to know that he was hanging in there, and we were honored to make a small dent in his life.
Sometimes it’s hard to convey the message in some of our stories. How does one express a lifetime of chaos, doubt, and failure? Joyce experienced all of these things in her journey through Narcolepsy. The comments to our telling of Joyce’s story conveyed the message: You’re not alone, you’re not crazy, and your perseverance is an inspiration.
We often receive notes and messages from the people that we help that thank us for what we do. We’re referred to as “angels”, “lifesavers”, and “heroes”. That is all very flattering but we sometimes come across someone who puts everything into perspective for us. Such is the case with Dennis.
Dennis is a bona-fide New York City Detective with over 20 years of experience on the beat. He went from a street cop to an undercover officer, and then received his Detective’s shield. He was in Manhattan on September 11, 2001 and spent several grueling months at Ground Zero as he and his comrades combed the wreckage for remains. He was then diagnosed with Pulmonary Hypertension.
Dennis’s story brought comments, encouragement (and some flirting!), from friends, PH sufferers, and cops with PH. People heard his story of courage from just across town in Long Island, from all over America, and from as far away as Scotland.
We wonder how many others there are out there like Dennis, Joyce, Matthew, Roberta, Meghan, and Justin? We’re sure that there are millions of you. And we plan on continuing to provide a voice for you. If you’re someone who is currently working with us, or someone who stumbled across our site, we’d love to hear from you. Contact us and let us share your story.
We empower patients who live with life threatening chronic diseases. The people in the stories that we’ve shared are the heroes.
Posted in Diseases, Featured, Uncategorized | Tagged Alpha 1, Contact Us, Huntington's, Infantile Spasms, narcolepsy, PF, PH | Leave a commentA Life With Narcolepsy
December 7, 2011 Joyce was still a child when she knew that something was wrong. Growing up in Rhode Island should have been idyllic, except that something was not quite right.
Joyce was still a child when she knew that something was wrong. Growing up in Rhode Island should have been idyllic, except that something was not quite right.
At the age of four she would see the clothes moving in the closet. It seemed that every night she would be screaming for her parents to come and get the monster hidden in the hangers. The only thing worse than that was the monster under her bed. That one would keep her awake by tickling her feet. Even in the summer heat, it was only by covering her feet with blankets that the tickle monster could be held at bay. Her parents would turn on the lights, shake out the clothes, and check under the bed.
“Go back to sleep,” they would tell her. “You’re having a nightmare.”
Even at a young age, she knew that it was something else. How could she be having a nightmare if she was still awake?
As Joyce got older, she found the closet monster replaced with colorful visions of dancing figures with fanciful faces and festive hats. The tickle monster has stayed for life.
Initially a poor student, it wasn’t until high school that Joyce realized that the more challenging her classes, the better her grades. She nodded off during boring lectures and struggled with her notes. Hours of homework and vigorous note taking covered up for her sleepiness and her reputation as the “absent-minded student”. For the first time in her life, she made the honor roll.
Joyce went on to college, but left. Her decision to leave wasn’t based on her struggles with study, but for love.
She married an Air Force man, and after several years in New Hampshire, spent several in the Philippines before landing in England. After the birth of a daughter, the couple saw the arrival of twin girls. Joyce found a job on the base in the NCO Club, and established a good network among the other wives.
She worked the second shift at the Club so that she could be there for the girls, and while she slept well, she found herself needing frequent naps. During morning coffee with the neighbors, she found herself nodding off. It was particularly inconvenient when she was in mid-sentence. The girls of the coffee group would laugh but were understanding. Living in a foreign country, working, raising three young daughters, and being a military wife added up.
The routine was broken after five years when she and her husband decided to split. She gathered the girls and returned to Rhode Island.
Joyce found a home for her family, and found two jobs that could make ends meet. An illness found her unable to work, and during her time off she discovered a program that would help her to return to school. She found herself at the Community College and began taking computer science courses. She began to again feel the effects of being a single mother, the toll of being a full time student, and began to nod off during boring lectures. She thought back to her younger days, she plowed ahead, and found herself on the dean’s list!
A chance phone call from the Rhode Island Job Opportunity and Training Agency found her taking a job as a programmer. She continued with classes, forged ahead with a promising career, and went about raising her girls. And she struggled.
She would start a project at work, and anxious to show it off to her supervisor, would pull up the code that she had worked so hard on. Changes that she had made would not be there! A program that she had debugged would still be full of glitches. Was someone playing tricks on her? She would have a distinct memory of working on a project and see it unfinished. Notes that she had meticulously taken became scribbles and unreadable.
Often, when her supervisor came to check on her, he would find her nodding off at her desk. The screen that was supposed to be full of computer code would evolve into shopping lists, reminders to pick up milk, or dissolve into gibberish.
Things were getting difficult at home as well. She was always tired, it seemed that the house was never clean, and cooking gave way to take-out. She began to have financial troubles. Bills that she had set aside to pay by a certain date were forgotten. Checks that she had written and sent out were found lying around weeks later. Was she irresponsible? Was she lazy? Was she an unfit mother?
After a lifetime of exhaustion, visions, and the “tickle-monster”, she went to a doctor who recommended a sleep study. It wasn’t a character flaw. It wasn’t stress. It wasn’t anxiety or the struggles of a single mother. It was Narcolepsy.
As her symptoms have worsened, Joyce has tried working shorter hours. One employer allowed her to keep a cot in a storage room. She has tried working from home. It has gotten harder to maintain a career when she can’t concentrate at a keyboard and her hands drop to her sides.
She has been in and out of the Disability radar. She has been on public assistance. She has spent the past decade trying different medicines and therapies. She has tried to be a mother, a grandmother, and a partner to those in relationships with her.
She works part-time now. She is working for the Narcolepsy Network. She still struggles with her disease, but she knows, she has Narcolepsy. The tickle-monster still visits, but he doesn’t scare her any more.
Posted in Diseases, Featured | Tagged narcolepsy, Narcolepsy Network | 8 CommentsA New Program for Narcolepsy Patients
October 11, 2011Caring Voice Coalition, Inc. (CVC), a non-profit organization that provides financial assistance and insurance advocacy for persons with specific chronic illnesses, is pleased to announce a new program to assist patients diagnosed with Narcolepsy.
Narcolepsy is a chronic sleep disorder characterized by excessive daytime sleepiness (EDS) in which a person experiences extreme fatigue and possibly falls asleep at inappropriate times, such as work or at school. Narcoleptics usually experience disturbed nocturnal sleep and an abnormal daytime sleep pattern, which is often confused with insomnia. Narcolepsy is often associated with cataplexy, a sudden loss of muscle tone often triggered by intense emotions, sleep paralysis and hypnogogic hallucinations. While medications often help to manage the signs and symptoms of Narcolepsy, there is currently no cure.
This announcement represents an expansion of CVC’s current programs which include Pulmonary Hypertension; Alpha-1 Antitrypsin Deficiency; Idiopathic Pulmonary Fibrosis; Chronic Granulomatous Disease; Complex Partial Seizures; Infantile Spasms and Huntington’s disease.
“CVC is very excited to offer this new program,” said Samantha Harris, Vice President of CVC. “We strive to improve the lives of our patients every day and look forward to expanding our assistance to the Narcolepsy Community.”
Tim Robertson, Senior Director of Patient Services, adds, “The rising costs of healthcare prevents many patients diagnosed with chronic illnesses from beginning or remaining on therapy. CVC’s new program will provide financial support to help qualified patients afford the out of pocket costs related to their prescribed therapy for Narcolepsy.”
About the Caring Voice Coalition:
Caring Voice Coalition, Inc. (CVC)is a national 501(c)(3) non-profit, charitable organization established in 2003 to provide financial, insurance education and patient support to individuals diagnosed with specific chronic or life-threatening diseases. CVC seeks to empower these patients by providing comprehensive programs delivered through a holistic approach by a staff of knowledgeable, dedicated and caring individuals.